Side effects are unintended and often undesirable reactions or consequences that occur as a result of taking medication, undergoing medical treatments, or engaging in certain activities. These effects are separate from the primary intended outcome and can range from mild discomfort to severe, life-threatening conditions. Side effects may manifest as physical symptoms, such as nausea, headaches, or skin rashes, or as psychological changes, including mood swings or cognitive impairment. The occurrence and severity of side effects can vary greatly among individuals, depending on factors such as age, overall health, and genetic predisposition. While some side effects may be temporary and resolve on their own, others may require additional medical intervention or necessitate discontinuation of the treatment or activity causing them.
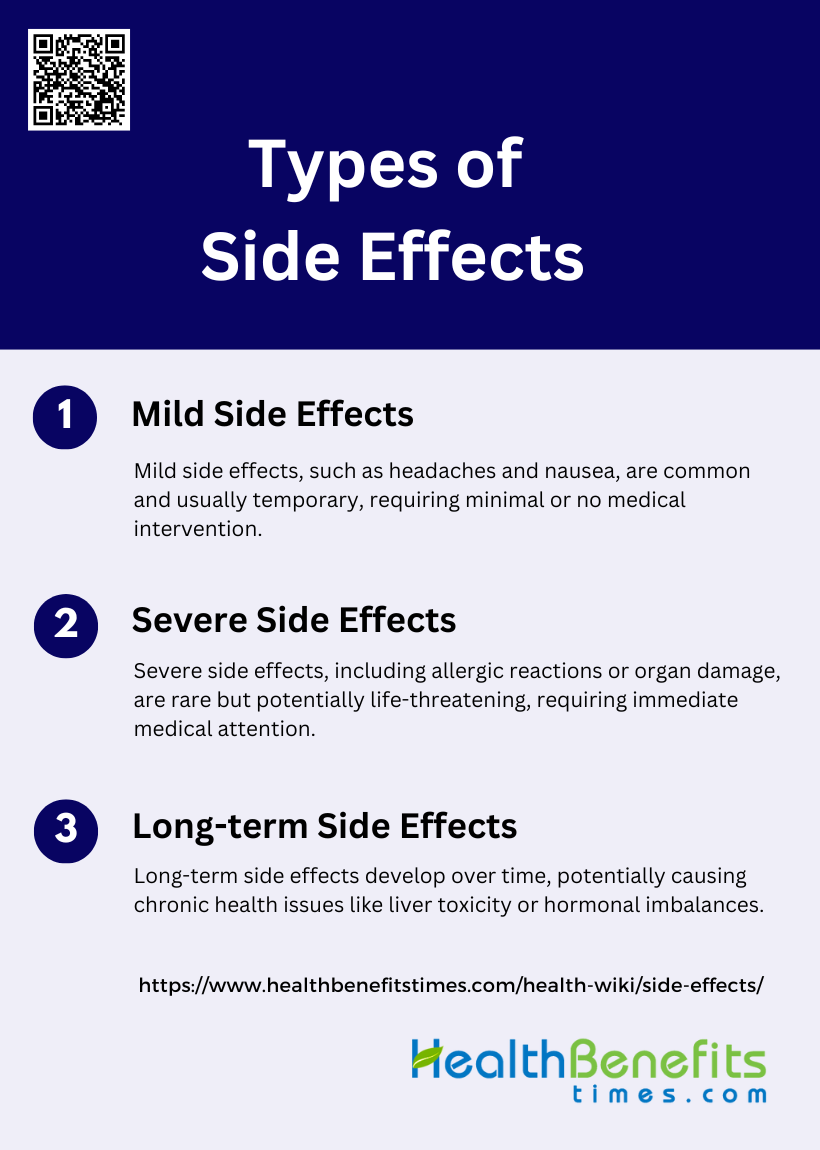
Types of Side Effects
When undergoing medical treatments or taking medications, individuals may encounter a range of side effects. These effects can vary widely in their intensity and duration, influencing the overall treatment experience. Below is a list of types of side effects:
1. Mild Side Effects
Mild side effects are common and generally manageable, often resolving on their own or with minimal intervention. Examples include nausea, headaches, and stomachaches. These effects are typically temporary and do not require significant medical intervention. For instance, in a study on children with ADHD treated with methylphenidate, common mild side effects included decreased appetite, insomnia, stomachaches, and headaches, which were generally mild and manageable. Similarly, intrathecal morphine therapy for chronic pain often results in mild side effects such as nausea, vomiting, and pruritus, which are dose-dependent and can be managed with appropriate treatment.
2. Severe Side Effects
Severe side effects are less common but can be life-threatening and require immediate medical attention. These include allergic reactions, organ damage, and severe respiratory depression. For example, some of the most severe adverse drug reactions are allergic in nature, involving mechanisms such as drug-specific IgE development and serum-sickness-like reactions. In the case of intrathecal morphine therapy, less common but severe side effects include respiratory depression and catheter tip inflammatory mass formation, which necessitate prompt medical intervention. Additionally, a small percentage of children on methylphenidate experienced severe side effects that warranted immediate discontinuation of the medication.
3. Long-term Side Effects
Long-term side effects develop over an extended period and can lead to chronic health issues. These include liver toxicity, hormonal imbalances, and other delayed adverse effects. Long-term intrathecal morphine therapy, for instance, can lead to chronic side effects such as urinary retention, constipation, sexual dysfunction, and edema, which are often dose-dependent and mediated by opioid receptors. These chronic side effects necessitate ongoing monitoring and management to mitigate their impact on the patient’s quality of life. Additionally, unpredictable adverse drug reactions, influenced by pharmacogenetic variations, can result in long-term health complications.
Common Causes of Side Effects
Medication-Induced Side Effects
Medication-induced side effects are a common concern in medical treatments, often leading to non-adherence and reduced quality of life. Chemotherapy, for instance, is known to cause a range of side effects, including cognitive deficiencies, fatigue, and neuropathy, which can persist long after treatment has ended. These side effects are often due to the neurotoxic effects of chemotherapeutic agents, which can damage both peripheral and central nervous systems. Additionally, the fear of side effects can exacerbate their perception, creating a nocebo effect that further complicates treatment adherence. Understanding these mechanisms is crucial for developing better management strategies to mitigate these adverse effects.
Side Effects from Treatments (e.g., Chemotherapy)
Chemotherapy is a cornerstone in cancer treatment but is notorious for its severe side effects, which can significantly impact patients’ quality of life. These side effects include DNA damage, which not only targets cancer cells but also harms healthy cells, leading to toxicities and accelerated aging. Common side effects include oral mucositis, gastrointestinal toxicity, hepatotoxicity, nephrotoxicity, and neurotoxicity. The neurotoxic complications can range from peripheral neuropathy to severe central neurotoxicity, such as cognitive deficits and encephalopathy. These adverse effects often necessitate dose reductions or even cessation of treatment, highlighting the need for effective management strategies.
Environmental Factors Leading to Side Effects
Environmental factors can also contribute to the side effects experienced during medical treatments. For instance, the induction of a pro-metastatic microenvironment by chemotherapy or radiotherapy is an often overlooked but significant issue. These treatments can cause toxic damage to various organs, leading to the upregulation of factors that attract cancer cells, thereby facilitating metastasis. Additionally, psychological factors such as negative expectations and pre-conditioning can exacerbate the perception of side effects, creating a nocebo effect that further burdens patients. Understanding these environmental and psychological factors is essential for developing comprehensive strategies to mitigate side effects and improve patient outcomes.
How to Identify and Manage Side Effects
Recognizing Side Effects
Understanding and identifying side effects is crucial for safe medication use. Reading labels and understanding potential reactions can help patients recognize side effects early. It is also important to know when to seek medical advice. Older patients, for example, often correctly identify side effects, but severe reactions can be missed, highlighting the need for professional consultation. Sharing information about side effects does not significantly increase their occurrence or negatively impact treatment compliance, so patients should be well-informed to actively participate in their care.
Managing Mild Side Effects
For managing mild side effects, home remedies or simple adjustments can often reduce discomfort. Patients should discuss any side effects with their healthcare provider to ensure they are managing them correctly and to rule out more serious issues. Open communication with healthcare providers allows for adjustments in medication or dosage, which can alleviate mild side effects without compromising the treatment’s effectiveness. This proactive approach helps in maintaining overall treatment adherence and patient well-being.
Managing Severe Side Effects
In cases of severe side effects, such as allergic reactions or breathing issues, immediate action is necessary. Patients should be aware of the steps to take in emergency situations, including contacting emergency services and informing healthcare providers about the reaction. Recognizing the signs of severe reactions early and knowing how to respond can prevent complications and ensure timely medical intervention. Education on emergency protocols and having a plan in place can significantly improve outcomes in such critical situations.
Preventing Side Effects
Managing and preventing side effects is a crucial aspect of any medical treatment plan. By taking proactive steps and staying informed, patients can significantly reduce the likelihood of experiencing adverse reactions. Below is a list of strategies to help prevent side effects effectively.
1. Follow Instructions Carefully
Adhering to prescribed medication regimens is crucial for preventing side effects and ensuring the effectiveness of treatment. Studies have shown that non-adherence to medication can lead to increased mortality and poor health outcomes. For instance, in the Prostate Cancer Prevention Trial, non-adherence was associated with higher mortality rates from unrelated conditions. Therefore, patients should follow their healthcare provider’s instructions meticulously, including dosage, timing, and any specific guidelines related to food or other medications. This careful adherence helps in minimizing the risk of adverse effects and maximizing the therapeutic benefits of the medication.
2. Communicate with Healthcare Providers
Effective communication with healthcare providers is essential for preventing side effects. Patients should discuss any concerns or side effects they experience with their doctors to adjust the treatment plan accordingly. For example, interventions that include counseling and regular follow-ups have been shown to improve medication adherence and treatment outcomes. By maintaining an open line of communication, patients can receive timely advice on managing side effects, adjusting dosages, or switching medications if necessary, thereby enhancing the overall effectiveness of the treatment and reducing the risk of adverse effects.
3. Be Informed
Being well-informed about the medications one is taking can significantly reduce the risk of side effects. Patients should educate themselves about the potential side effects of their medications and how to manage them. Studies have shown that informing patients about the adverse effects of treatment does not negatively impact adherence. In fact, understanding the risks and benefits can empower patients to take proactive steps in managing their health, such as recognizing early signs of side effects and seeking medical advice promptly. This knowledge can also help in making informed decisions about their treatment options.
4. Make Lifestyle Adjustments
Lifestyle adjustments can play a significant role in preventing side effects and improving overall health outcomes. For instance, lifestyle modifications such as diet and exercise are recommended alongside medication for the prevention of cardiovascular diseases. These changes can enhance the effectiveness of the medication and reduce the likelihood of side effects. Studies have shown that interventions combining medication adherence with lifestyle modifications can lead to better health outcomes, such as reduced blood pressure and cholesterol levels. Therefore, patients should consider incorporating healthy lifestyle habits as part of their treatment plan.
5. Take Precautions
Taking necessary precautions can help in minimizing the risk of side effects. This includes avoiding activities or substances that may interact negatively with the medication. For example, patients should be aware of potential drug interactions and avoid consuming alcohol or certain foods that may exacerbate side effects. Additionally, using tools like electronic pillboxes or mobile phone reminders can help in maintaining adherence to the medication regimen. By taking these precautions, patients can reduce the risk of adverse effects and ensure the safe and effective use of their medications.
6. Monitor and Report
Regular monitoring and reporting of any side effects to healthcare providers are crucial for preventing serious complications. Patients should keep track of their symptoms and report any unusual or severe side effects immediately. Studies have highlighted the importance of self-monitoring and regular follow-ups in improving medication adherence and managing side effects. By actively monitoring their health and communicating with their healthcare providers, patients can receive timely interventions to address any issues, thereby preventing the escalation of side effects and ensuring better health outcomes.
7. Consider Timing and Dosage
The timing and dosage of medication can significantly impact its effectiveness and the likelihood of side effects. Patients should adhere to the prescribed schedule and dosage to avoid underdosing or overdosing, which can lead to adverse effects. Research has shown that adherence to the prescribed dosing regimens is essential for achieving the desired therapeutic outcomes and preventing complications. For instance, in the management of hypertension, consistent adherence to the prescribed medication schedule is crucial for controlling blood pressure and preventing resistant hypertension. Therefore, patients should pay close attention to the timing and dosage of their medications as instructed by their healthcare providers.
FAQs
1. Can side effects develop after long-term use of a medication?
Yes, certain medications can cause side effects that only appear after prolonged use. These may include issues like liver or kidney damage, hormonal imbalances, or chronic fatigue. It’s important to regularly monitor your health and discuss any changes with your healthcare provider over time.
2. Are side effects always related to the dosage of the medication?
While many side effects are dose-dependent, meaning they worsen with higher doses, others can occur regardless of the amount of medication taken. For example, allergic reactions or rare genetic predispositions can cause side effects even at low doses.
3. Can lifestyle choices influence the severity of side effects?
Yes, factors like diet, exercise, alcohol consumption, and stress levels can impact the severity of medication side effects. For instance, consuming alcohol with certain medications may exacerbate side effects like dizziness or liver toxicity.
4. How do I know if a side effect requires immediate medical attention?
While mild side effects like headaches or nausea may not require urgent care, severe symptoms such as difficulty breathing, swelling, or severe chest pain warrant immediate medical intervention. Always consult your healthcare provider to understand which side effects are urgent.
5. Can side effects be temporary or do they last as long as I’m taking the medication?
Some side effects are temporary and subside after your body adjusts to the medication, while others may persist as long as you’re on the treatment. In some cases, side effects can even continue after stopping the medication, especially with long-term treatments.
6. What is the role of genetics in experiencing side effects?
Genetics can play a major role in how your body metabolizes medications, making you more or less likely to experience certain side effects. Pharmacogenetics, a field of study, helps tailor treatments based on your genetic makeup to minimize side effects.
7. Can I prevent side effects by switching medications?
In some cases, switching to a different medication within the same drug class or trying an alternative treatment might help reduce side effects. However, this should only be done under the guidance of a healthcare provider.
8. Can side effects vary depending on the method of medication delivery?
Yes, side effects can differ based on whether a medication is taken orally, injected, or applied topically. For instance, topical treatments may lead to skin irritation, while oral medications might cause gastrointestinal issues.
9. Do over-the-counter medications have fewer side effects than prescription medications?
Over-the-counter (OTC) medications can still cause side effects, even if they are generally considered safer than prescription medications. Some OTC drugs, like pain relievers, can cause gastrointestinal issues or allergic reactions when misused or taken long-term.
10. Can taking multiple medications increase the likelihood of side effects?
Yes, drug interactions from taking multiple medications can heighten the risk of side effects. Always inform your healthcare provider about all the medications, supplements, and herbal remedies you are taking to minimize these risks.