A laceration is a type of wound characterized by a tear or irregular cut in the skin, typically caused by trauma or injury. These wounds can vary in severity, ranging from superficial cuts to deep gashes that may affect underlying tissues, muscles, or even bones. Lacerations are common injuries in various settings, including sports like ice hockey, where they frequently occur on the face due to contact with sticks or pucks. The treatment of lacerations often involves cleaning the wound, closing it with sutures or other methods, and monitoring for potential complications such as infection. Factors that can increase the risk of infection in lacerations include diabetes, wound contamination, length greater than 5 cm, and location on the lower extremity.
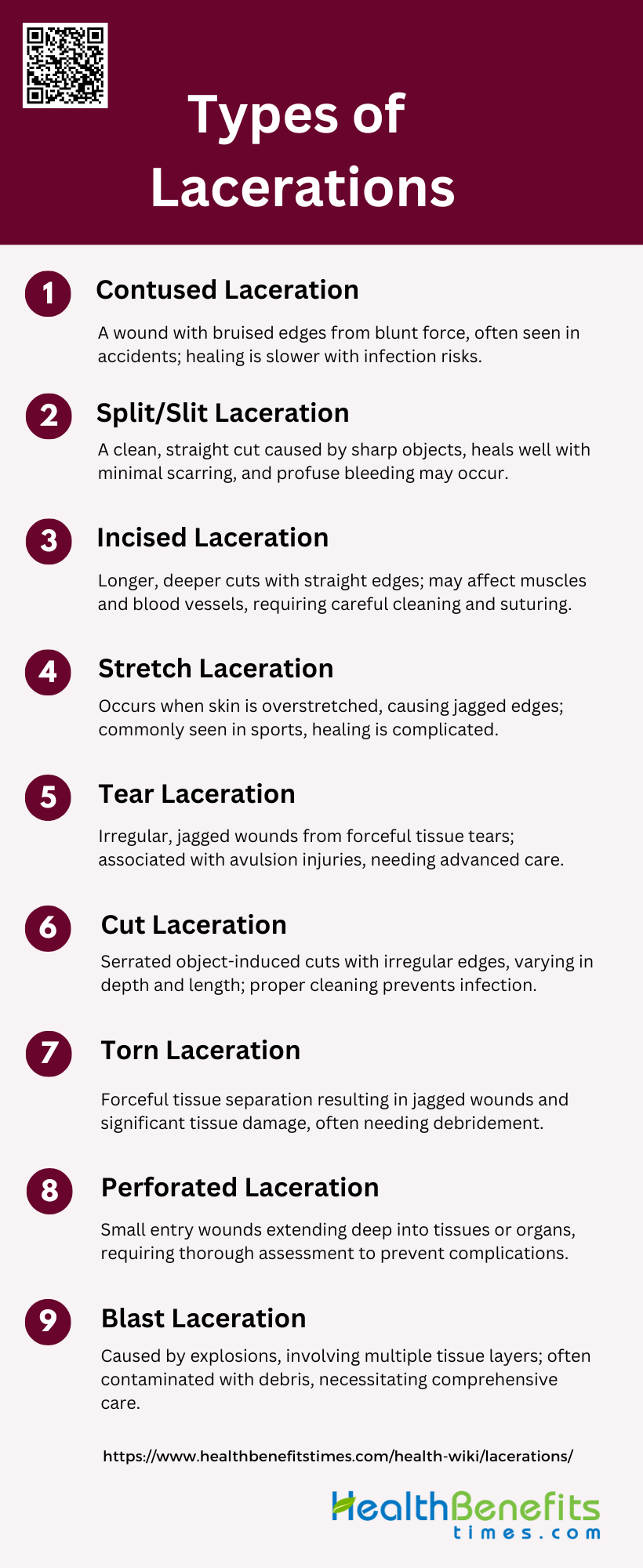
Types of Lacerations
Lacerations are injuries that result in the tearing or cutting of skin and tissue, often caused by sharp or blunt trauma. They can vary in depth, severity, and treatment requirements. Below is a list of different types of lacerations:
1. Contused Laceration
A contused laceration is a type of wound that combines the characteristics of both a contusion (bruise) and a laceration (cut). This injury occurs when blunt force trauma causes the skin to split open, resulting in a ragged, irregular wound with bruised edges. Contused lacerations are often seen in accidents involving heavy objects or falls onto hard surfaces. The tissue surrounding the wound is typically damaged and bruised, which can lead to slower healing and a higher risk of infection. These injuries are common in areas with thin skin overlying bony prominences, such as the scalp or shin.
2. Split/Slit Laceration
Split or slit lacerations are characterized by a clean, straight cut through the skin and underlying tissues. These injuries are typically caused by sharp objects with a thin edge, such as knives, razors, or glass shards. The wound edges are usually smooth and well-defined, with minimal tissue damage surrounding the cut. Split lacerations tend to bleed more profusely than other types due to the clean separation of blood vessels. They generally heal well with proper treatment, often resulting in a thin, linear scar.
3. Incised Laceration
An incised laceration is similar to a split laceration but is typically longer and may be deeper. These wounds are caused by sharp objects and are characterized by clean, straight edges with minimal tissue damage around the wound. Incised lacerations can vary in depth and length, potentially affecting underlying structures such as muscles, tendons, or blood vessels. They often require careful cleaning and may need sutures or other closure methods to promote proper healing. Incised lacerations are common in workplace accidents, particularly in industries involving sharp tools or machinery.
4. Stretch Laceration
Stretch lacerations occur when the skin is stretched beyond its elastic limit, causing it to tear. These injuries are often seen in areas where the skin is under tension, such as over joints or in regions with significant subcutaneous fat. Stretch lacerations typically have irregular, jagged edges and may be accompanied by underlying tissue damage. They are common in high-impact sports, motor vehicle accidents, and falls. Healing of stretch lacerations can be more complicated due to the nature of the tissue damage, and they may require specialized wound care to minimize scarring.
5. Tear Laceration
Tear lacerations are characterized by irregular, jagged wound edges and are often associated with avulsion injuries. These wounds occur when tissue is forcefully torn away from its attachment, resulting in a ragged appearance. Tear lacerations can involve multiple layers of tissue and may be accompanied by significant tissue loss. They are commonly seen in accidents involving machinery, animal bites, or severe falls. Due to their irregular nature, tear lacerations often require careful debridement and may need advanced wound closure techniques to achieve optimal healing.
6. Cut Laceration
Cut lacerations are similar to incised lacerations but are typically caused by less sharp objects or those with a serrated edge. These wounds may have slightly more irregular edges compared to clean incised lacerations. Cut lacerations can vary in depth and length, potentially affecting underlying structures. They are often seen in accidents involving household items, tools, or broken glass. Proper cleaning and closure of cut lacerations are essential to prevent infection and promote optimal healing.
7. Torn Laceration
Torn lacerations are characterized by irregular, ragged edges and are often associated with significant tissue damage. These injuries occur when skin and underlying tissues are forcefully pulled apart, resulting in a jagged wound. Torn lacerations can be accompanied by tissue loss and may involve multiple layers of skin, fat, and muscle. They are commonly seen in severe accidents, explosions, or animal attacks. Due to the extensive tissue damage, torn lacerations often require careful debridement and may need advanced wound closure techniques or even skin grafts for proper healing.
8. Perforated Laceration
Perforated lacerations are characterized by a small entry wound that extends deeper into the underlying tissues or body cavities. These injuries are typically caused by sharp, pointed objects such as nails, needles, or bullets. Perforated lacerations can be particularly dangerous as they may involve damage to internal organs or structures that are not immediately visible. They require thorough assessment and may need imaging studies to determine the full extent of the injury. Treatment often involves careful exploration of the wound and may require surgical intervention to address any internal damage.
9. Blast Laceration
Blast lacerations are a specific type of injury caused by explosions or high-pressure events. These lacerations are often accompanied by other blast-related injuries such as burns, contusions, and internal organ damage. Blast lacerations can vary widely in severity and appearance, ranging from small superficial cuts to deep, extensive tissue damage. They may be contaminated with debris or foreign bodies, increasing the risk of infection. Treatment of blast lacerations often requires a multidisciplinary approach, addressing not only the wound itself but also potential associated injuries and complications.
Causes of Lacerations
Lacerations are common injuries that occur when the skin and underlying tissues are torn or cut. They can result from a variety of causes, each presenting unique challenges in terms of treatment and healing. Below is a list of common causes of lacerations:
1. Blunt Force Trauma
Blunt force trauma is a significant cause of lacerations, often resulting from impacts with objects that have substantial mass and velocity. These injuries can produce irregular margins and may involve bridging by more resilient tissues. Common scenarios include motor vehicle accidents, falls, and assaults. The skin and underlying tissues may exhibit contusions, abrasions, and lacerations, with the latter often having irregular, jagged edges. The thoracic and abdominal regions are particularly susceptible, with potential for internal injuries such as rib fractures and organ lacerations. Understanding the biomechanics of blunt force trauma is crucial for accurate diagnosis and effective treatment.
2. Sharp Objects
Lacerations caused by sharp objects, such as knives, glass, or metal, are typically characterized by clean, straight edges. These injuries are classified into stab, incised, and chop wounds, and are less frequent than blunt-force injuries. Sharp-force trauma can result in significant blood loss and may lead to hypovolemic shock, pneumothorax, or asphyxiation if vital structures are compromised. Accurate documentation and examination of these wounds are essential for determining the instrument used and the force applied. These injuries often occur in contexts of social violence, accidents, or specific rituals, necessitating thorough forensic investigation.
3. Accidents and Injuries
Accidental injuries are a common cause of lacerations, often occurring during everyday activities or recreational pursuits. These injuries can result from falls, collisions, or mishandling of tools and equipment. The nature of the laceration—whether caused by blunt force or sharp objects—depends on the circumstances of the accident. For instance, motor vehicle accidents frequently result in blunt force trauma, while mishandling sharp tools can lead to clean cuts. Effective management of these injuries involves proper wound cleaning, tetanus prophylaxis, and sometimes antibiotic administration to prevent infection.
4. Explosions and Blast Injuries
Explosions and blast injuries can cause complex lacerations due to the combination of blunt force and sharp object trauma. The high-energy impact from an explosion can result in extensive tissue damage, including deep lacerations, contusions, and abrasions. These injuries are often compounded by the presence of foreign materials such as shrapnel, which can introduce additional complications. The management of blast injuries requires a multidisciplinary approach to address both the immediate and long-term consequences, including infection control and reconstructive surgery.
5. Grinding Forces
Grinding forces, often encountered in industrial settings, can cause severe lacerations characterized by irregular, jagged edges. These injuries occur when body parts come into contact with rotating machinery or abrasive surfaces, leading to extensive tissue damage. The nature of grinding injuries often necessitates thorough debridement to remove devitalized tissue and prevent infection. Protective measures and safety protocols are essential in environments where grinding forces are prevalent to minimize the risk of such injuries.
6. Crush Injuries
Crush injuries result from the application of significant force over a prolonged period, leading to extensive tissue damage and lacerations. These injuries are common in industrial accidents, natural disasters, and vehicular collisions. The pressure exerted can cause deep lacerations, contusions, and even fractures. Crush injuries often lead to complications such as compartment syndrome and require immediate medical intervention to prevent long-term damage. Effective management includes relieving pressure, debridement, and monitoring for signs of infection 5.
7. Animal Attacks
Lacerations from animal attacks are typically caused by bites or scratches, resulting in irregular, jagged wounds. These injuries can vary in severity depending on the size and type of the animal involved. Animal bites pose a high risk of infection due to the presence of bacteria in the animal’s mouth. Immediate and thorough cleaning of the wound, along with appropriate antibiotic prophylaxis, is crucial to prevent infection. In some cases, rabies prophylaxis may also be necessary. Accurate documentation and reporting of animal attacks are important for public health and safety.
8. Medical Procedures
Lacerations can also occur as a result of medical procedures, either accidentally or as part of surgical interventions. These iatrogenic injuries may arise from the use of sharp instruments or during the handling of tissues. While most medical lacerations are intentional and controlled, accidental lacerations can complicate the patient’s recovery process. Proper surgical techniques, careful handling of instruments, and adherence to safety protocols are essential to minimize the risk of such injuries. Post-procedural care includes monitoring for signs of infection and ensuring proper wound healing.
Sign and symptoms of Lacerations
Lacerations are cuts or tears in the skin or tissue, often caused by blunt trauma or sharp objects. The severity of lacerations can vary, and the signs and symptoms generally depend on the depth, size, and location of the injury. Here are the common signs and symptoms of lacerations:
1. Visible Tear or Cut: The skin or tissue will have a visible tear or open wound. The edges of the wound may be jagged or smooth, depending on the cause.
2. Bleeding: Mild to severe bleeding can occur depending on the depth and location of the laceration. Superficial lacerations may have minimal bleeding, while deeper wounds involving blood vessels can lead to significant blood loss.
3. Pain: Pain at the site of the injury is common, ranging from mild to intense, depending on the depth of the cut and involvement of nerve endings.
4. Swelling: Swelling around the laceration can occur due to inflammation and injury to surrounding tissues.
5. Redness: The area around the laceration may appear red and inflamed as the body responds to the injury.
6. Bruising: Bruising (discoloration around the wound) can occur if there is damage to underlying blood vessels.
7. Decreased Function: If the laceration occurs near a joint or muscle, there may be limited movement or function in the affected area due to pain or damage to muscles, tendons, or ligaments.
8. Numbness: If the laceration damages nerves, there may be numbness or tingling around the wound.
9. Infection Signs (if not treated properly)
- Pus or drainage from the wound
- Increased redness, warmth, or swelling around the site
- Fever or general malaise
10. Scarring: After healing, a scar may form at the site, especially if the wound was deep or improperly treated.
11. Shock (in severe cases): In cases of severe blood loss or traumatic injury, the person may experience signs of shock, such as pale skin, rapid heartbeat, and confusion.
Risks and Complications of Lacerations
Lacerations, or cuts, are common injuries that can lead to various complications if not properly managed. Understanding these risks is crucial for effective treatment and prevention. Here are some key risks and complications associated with lacerations:
1. Infection Risk
Lacerations are highly susceptible to infections, especially when dirt, bacteria, and debris are present in the wound. Studies have shown that contaminated lacerations significantly increase the risk of infection. For instance, one study found that contaminated lacerations had a relative risk (RR) of 2.0 for developing infections compared to clean wounds. Additionally, factors such as diabetes and the location of the laceration (e.g., lower extremities) further elevate the infection risk. Effective wound management, including thorough cleaning and timely closure, is crucial to minimize these risks.
2. Scarring
The potential for scarring from lacerations depends on various factors, including the depth of the wound and the treatment method used. A study comparing absorbable and nonabsorbable sutures in pediatric lacerations found no significant difference in long-term cosmetic outcomes, suggesting that proper suture technique can mitigate scarring risks. However, infections and improper wound closure can lead to unsightly and dysfunctional scars, emphasizing the importance of appropriate wound care. The use of tissue adhesives has also been shown to improve cosmetic outcomes by providing a more aesthetically pleasing scar.
3. Damage to Deeper Tissues
Lacerations can extend beyond the skin, affecting deeper tissues such as nerves, blood vessels, and muscles. This can lead to complications like loss of sensation, impaired blood flow, and reduced muscle function. For example, a study on dermatome-induced lacerations in burn surgery highlighted that most lacerations extended to subcutaneous tissue, although neurovascular injuries were rare. Proper assessment and management of lacerations are essential to identify and treat any damage to deeper tissues, thereby preventing long-term complications.
4. Excessive Bleeding
Deep lacerations can cause significant bleeding, posing a risk of hemorrhage. This is particularly concerning in areas with rich blood supply or in patients with bleeding disorders. For instance, cervical lacerations during childbirth can lead to substantial blood loss, necessitating immediate medical intervention. Effective hemostasis techniques, such as pressure application, suturing, and the use of hemostatic agents, are critical in managing excessive bleeding and preventing further complications.
5. Loss of Function
The location of a laceration can significantly impact the risk of functional loss. Lacerations on joints, tendons, or muscles can impair movement and strength, leading to long-term disability. For example, lacerations on the lower extremities are associated with a higher risk of infection and poor cosmetic outcomes, which can further contribute to functional impairment. Early and appropriate intervention, including surgical repair and physical therapy, is essential to restore function and prevent permanent disability.
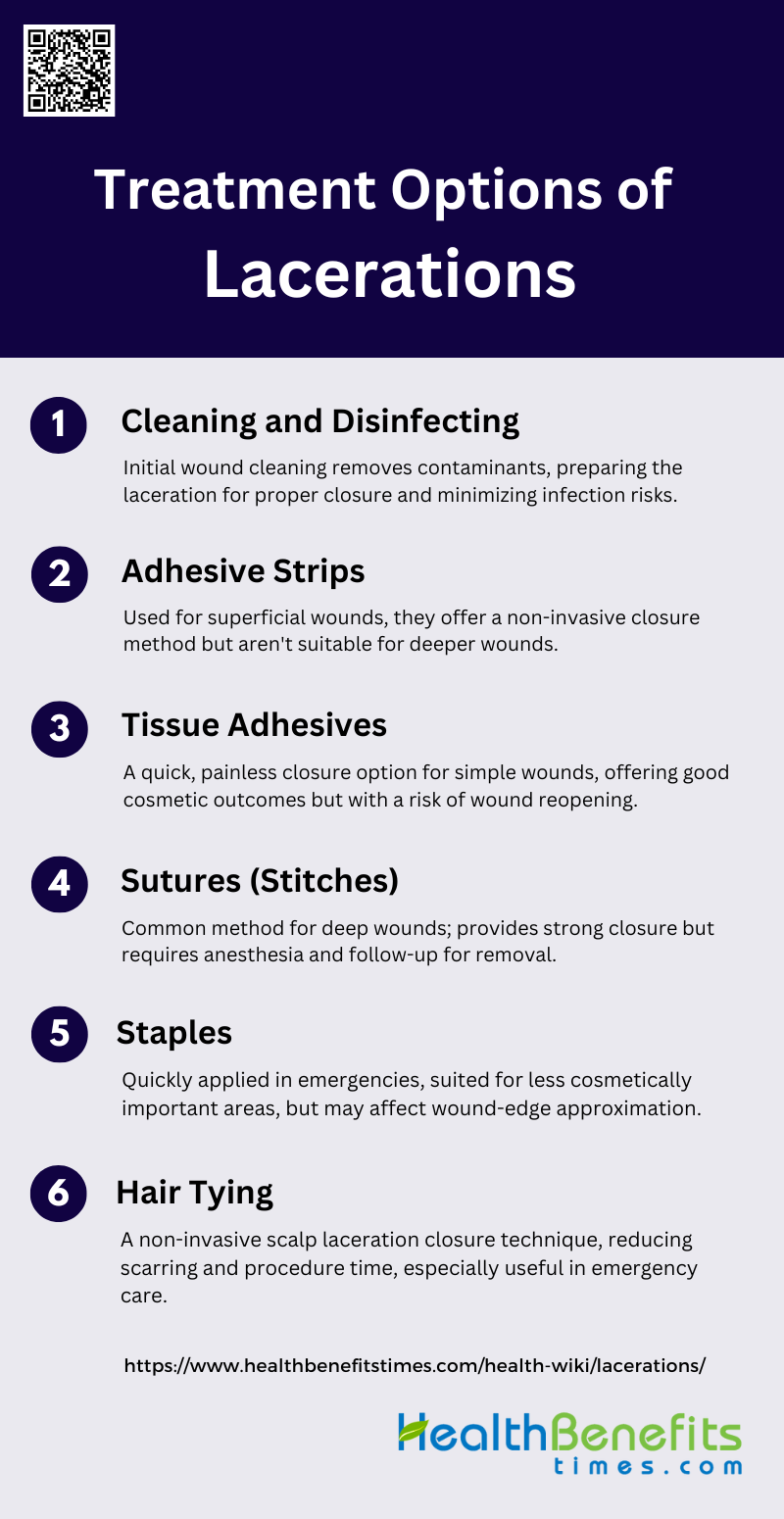
Treatment Options of Lacerations
Treating lacerations effectively is essential to ensure proper healing and minimize complications. Various treatment options are available, each suited to different types and severities of cuts. Below are some common methods used to treat lacerations:
1. Cleaning and Disinfecting
Cleaning and disinfecting a laceration is a critical first step in wound management to prevent infection and promote healing. The surrounding intact skin, rather than the wound itself, should be disinfected to avoid further contamination. Hair around the wound should be clipped to 1-2 mm above the skin using scissors or clippers, as shaving with a razor can damage hair follicles and increase infection risk. Irrigation with solutions such as Ringer’s, normal saline, or distilled water is essential to remove debris and contaminants. Following irrigation, debridement of contaminated and devitalized tissue is performed to prepare the wound for closure.
2. Adhesive Strips
Adhesive strips, such as Steri-Strips, are a non-invasive option for closing superficial or partial-thickness lacerations. They are particularly useful for wounds that are not subject to significant tension. Adhesive strips are easy to apply, cause minimal discomfort, and do not require follow-up visits for removal. However, they are not suitable for deeper or highly mobile areas where the wound edges are under considerable tension. Studies have shown that adhesive strips can be effective in reducing infection rates and scarring when used appropriately.
3. Tissue Adhesives
Tissue adhesives, like 2-octylcyanoacrylate, offer a quick and less painful alternative to sutures and staples for closing simple, low-tension lacerations. They are particularly advantageous in pediatric and emergency settings due to their ease of use and reduced procedure time. Tissue adhesives do not require follow-up visits for removal, which enhances patient convenience. Studies have demonstrated that tissue adhesives provide comparable cosmetic outcomes to traditional methods, with the added benefits of decreased pain and shorter application times. However, there is a slightly increased risk of wound dehiscence with tissue adhesives, which should be considered when choosing the closure method.
4. Sutures (Stitches)
Suturing is the most common method for closing lacerations, offering precise wound-edge approximation and strong closure, which is essential for wounds under significant tension. Various suturing techniques, such as simple, running, and mattress sutures, can be employed depending on the wound’s location and characteristics. Sutures are particularly effective for deeper lacerations and areas subject to movement. While suturing provides excellent cosmetic outcomes and reduces infection risk, it requires local anesthesia, which can be painful, and follow-up visits for suture removal.
5. Staples
Staples are a fast and effective method for closing lacerations, especially on the scalp, torso, and extremities. They are particularly useful in emergency settings due to their rapid application. However, staples do not offer the meticulous wound-edge approximation that sutures provide, which can affect cosmetic outcomes. Staples are best suited for linear lacerations in areas where cosmetic appearance is less of a concern. They also require follow-up visits for removal, similar to sutures.
6. Hair Tying
The hair apposition technique (HAT) is a novel method for closing scalp lacerations by twisting and securing hair strands on either side of the wound with tissue adhesive. This technique is particularly advantageous as it avoids the need for shaving, suturing, or staple removal, making it less invasive and more comfortable for patients. Studies have shown that HAT results in fewer complications, less scarring, and shorter procedure times compared to traditional suturing. It is highly accepted by patients and has become a preferred method for suitable scalp lacerations.
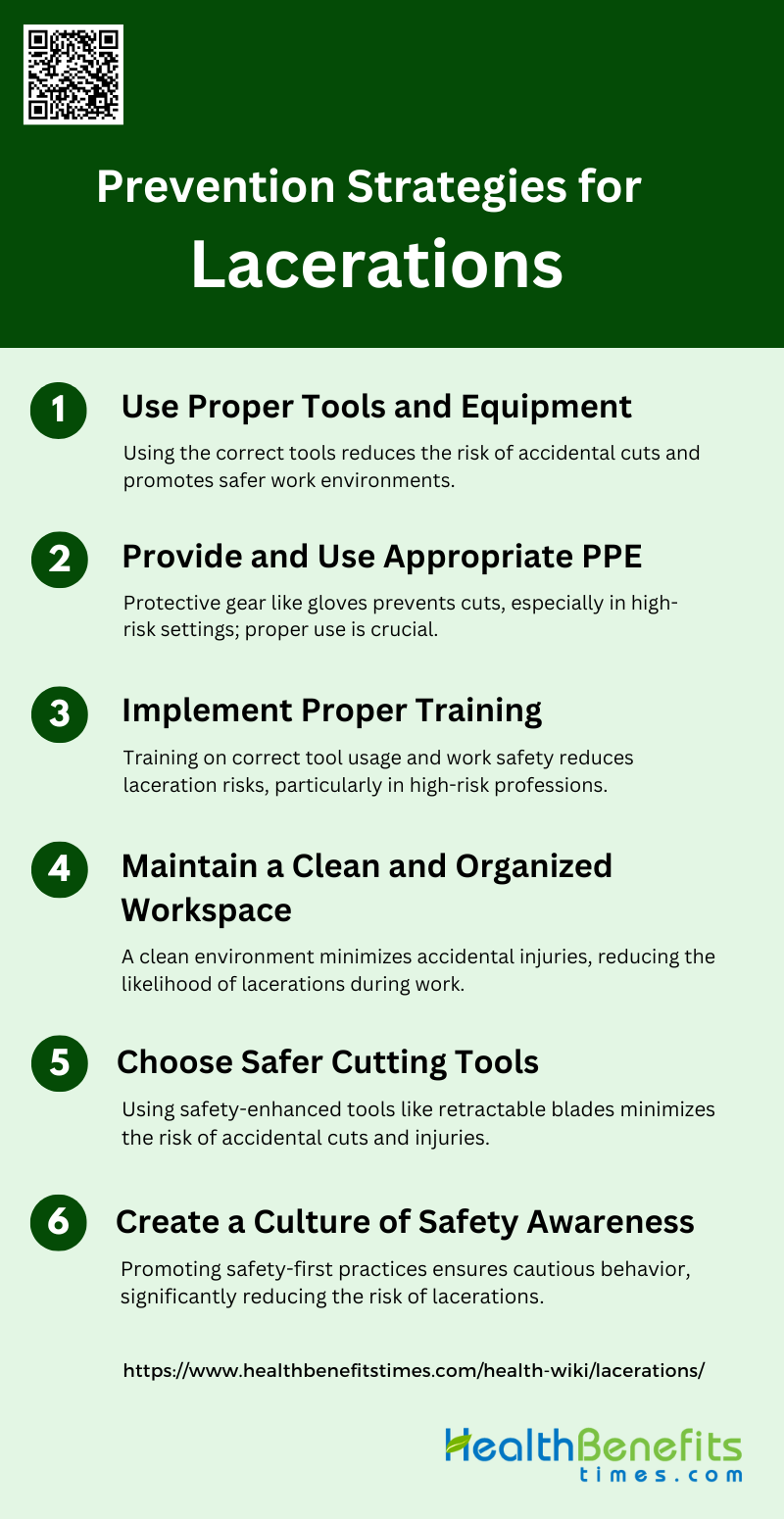
Prevention Strategies for Lacerations
Preventing lacerations is crucial in maintaining a safe and efficient work environment. By implementing effective strategies, the risk of cuts and injuries can be significantly reduced. Here are some key prevention strategies to consider:
1. Use Proper Tools and Equipment
Using the correct tools and equipment is essential in preventing lacerations. Proper tools ensure that tasks are performed efficiently and safely, reducing the risk of accidental cuts. For instance, the use of tissue adhesives has significantly improved wound closure options, minimizing the risk of infection and promoting better healing outcomes. Additionally, choosing the right cutting tools, such as those with safety features, can prevent accidental injuries. Ensuring that all equipment is well-maintained and suitable for the task at hand is a fundamental step in laceration prevention.
2. Provide and Use Appropriate PPE
Personal Protective Equipment (PPE) plays a crucial role in preventing lacerations, especially in high-risk environments. Proper use of PPE, such as gloves, can protect against cuts and abrasions. Studies have shown that nonsterile gloves are as effective as sterile gloves in preventing wound infections during laceration repair, highlighting the importance of using appropriate PPE. Additionally, best-evidence practice strategies emphasize the need for cleaning, moisturizing, and using prophylactic dressings to prevent skin damage related to PPE use among healthcare workers. Ensuring that PPE is used correctly and consistently can significantly reduce the risk of lacerations.
3. Implement Proper Training
Proper training is essential for preventing lacerations. Training programs should focus on the correct use of tools, equipment, and PPE, as well as safe work practices. For example, training healthcare workers in techniques such as perineal massage and warm compresses can reduce the incidence of severe perineal lacerations during childbirth. Additionally, educating workers on the importance of maintaining a clean and organized workspace can further minimize the risk of injuries. Continuous training and education ensure that all workers are aware of the best practices for preventing lacerations.
4. Maintain a Clean and Organized Workspace
A clean and organized workspace is vital for preventing lacerations. Cluttered and dirty work areas can increase the risk of accidental cuts and injuries. Proper wound management, including maintaining a sterile environment, is crucial for preventing infections and ensuring optimal healing. Additionally, organizing tools and equipment in a systematic manner can reduce the likelihood of accidental injuries. Ensuring that the workspace is regularly cleaned and organized can create a safer environment and reduce the risk of lacerations.
5. Choose Safer Cutting Tools
Choosing safer cutting tools is a proactive approach to preventing lacerations. Tools with safety features, such as retractable blades or safety guards, can significantly reduce the risk of accidental cuts. For instance, the use of tissue adhesives and wound adhesive strips in low-tension skin areas has been shown to be effective in achieving optimal cosmetic results without increasing the risk of infection. By selecting tools designed with safety in mind, the likelihood of lacerations can be minimized, promoting a safer working environment.
6. Create a Culture of Safety Awareness
Creating a culture of safety awareness is essential for preventing lacerations. Encouraging a safety-first mindset among workers can lead to more cautious and mindful behavior. For example, midwives and obstetricians can use techniques such as perineal massage and warm compresses to prevent perineal lacerations, considering women’s preferences and experiences. Promoting open communication about safety concerns and providing regular training on best practices can reinforce the importance of safety. By fostering a culture where safety is prioritized, the risk of lacerations can be significantly reduced.
Potential Complications of lacerations
Lacerations, while common, can lead to various complications if not properly managed. Understanding these potential issues is essential for effective treatment and prevention of further harm. Below are some of the key complications that can arise from lacerations:
1. Bleeding and Infection
Lacerations often present a significant risk of bleeding and infection, particularly if not managed properly. Immediate and effective wound care is crucial to minimize these risks. Studies have shown that mismanagement of lacerations can lead to wound infections, which prolong recovery and may result in unsightly and dysfunctional scars. Factors such as wound contamination, diabetes, and the location of the laceration (e.g., lower extremities) significantly increase the risk of infection. Proper cleaning, timely closure, and appropriate use of antibiotics are essential to prevent these complications. Additionally, the use of tissue adhesives has been found to reduce pain and procedure time, although they may slightly increase the risk of wound dehiscence.
2. Tissue Damage
Tissue damage is a common complication associated with lacerations, particularly when the injury involves deeper layers of skin, muscles, or nerves. The extent of tissue damage can significantly affect the healing process and the final cosmetic outcome. Incomplete wound edge apposition and the use of electrocautery have been associated with suboptimal cosmetic results and increased risk of infection. Moreover, lacerations involving significant tissue trauma are more likely to result in poor wound healing and increased scarring. Effective wound management, including proper debridement and careful suturing, is essential to minimize tissue damage and promote optimal healing.
3. Wound Closure Issues
Wound closure is a critical aspect of laceration management, and improper closure can lead to several complications. Techniques such as suturing, stapling, and the use of tissue adhesives each have their advantages and limitations. For instance, tissue adhesives are less painful and quicker to apply but may have a higher risk of dehiscence compared to traditional sutures. The choice of closure method should be based on the wound’s characteristics, including its location, size, and tension. Studies have shown that absorbable sutures can provide good long-term cosmetic outcomes without increasing the risk of infection or dehiscence. However, meticulous technique and appropriate material selection are crucial to ensure successful wound closure and minimize complications.
4. Scarring
Scarring is a common concern following laceration repair, and the goal is to achieve a functional and aesthetically pleasing scar. Factors such as the method of wound closure, the presence of infection, and the extent of tissue damage can significantly influence the final appearance of the scar. Studies have shown that tissue adhesives and absorbable sutures can provide comparable cosmetic outcomes to traditional sutures, with some evidence suggesting slightly better results with absorbable sutures. Additionally, techniques like the hair apposition technique (HAT) for scalp lacerations have been found to result in less scarring and fewer complications compared to standard suturing. Proper wound care and follow-up are essential to minimize scarring and achieve the best possible cosmetic outcome.
5. Healing Abnormalities
Healing abnormalities, such as delayed healing, hypertrophic scars, and keloids, can occur following laceration repair. Factors contributing to these abnormalities include infection, poor wound closure, and the patient’s overall health status. Elderly patients, in particular, may experience prolonged healing times and higher complication rates, as seen in studies of pretibial lacerations. Proper wound management, including timely and appropriate closure, infection prevention, and regular follow-up, is crucial to minimize healing abnormalities. Additionally, understanding patient-specific factors, such as underlying health conditions and the location of the laceration, can help tailor the treatment approach to promote optimal healing.
FAQs
1. Can lacerations heal without medical intervention?
Yes, minor lacerations can sometimes heal on their own, especially if the wound is clean and not too deep. However, medical intervention is often recommended to prevent infection, especially if the wound is large, deep, or in an area prone to movement. It’s important to clean and monitor the wound to ensure proper healing.
2. What are the signs that a laceration needs stitches?
Lacerations that are deeper than 1/4 inch, have jagged edges, or are located on areas of the body where movement is frequent (like joints) typically require stitches. If the wound continues to bleed after applying pressure, or if muscle, fat, or bone is visible, it should be seen by a healthcare professional for stitches.
3. How soon after a laceration should I seek medical attention?
It’s best to seek medical attention within 6 to 8 hours after a laceration occurs to reduce the risk of infection. Delays longer than 12 to 24 hours may increase the risk of complications and make it more difficult to close the wound properly.
4. What is the role of tetanus shots in laceration treatment?
If you suffer a laceration, particularly one that was caused by a rusty object or occurred outdoors, you may need a tetanus shot if your last vaccination was more than 10 years ago. Tetanus is a bacterial infection that can cause serious complications, and it is important to ensure you are up to date on your immunizations after certain injuries.
5. Can lacerations result in permanent numbness?
Yes, if a laceration damages nerves, especially in areas like the hands, face, or feet, there may be permanent numbness or tingling. Nerve damage can also affect mobility if the injury is severe. Early medical evaluation and treatment can sometimes prevent permanent damage.
6. What should I do if a laceration reopens after being treated?
If a treated laceration reopens, apply pressure to stop any bleeding and keep the area clean. You should contact your healthcare provider, as the wound may need additional closure methods such as stitches or adhesives, especially if it reopens due to infection or tension in the area.
7. Are there ways to minimize scarring after a laceration?
To minimize scarring, follow proper wound care instructions, including keeping the wound clean, avoiding direct sun exposure, and applying moisturizing ointments. Once the wound is healed, you can use silicone gels or sheets to improve the appearance of scars. Some people may also consider laser treatments or scar revision surgery for larger scars.
8. Is it normal for a laceration to itch during healing?
Yes, it’s common for lacerations to itch as they heal. Itching is a natural part of the healing process, indicating new skin formation. However, avoid scratching the area, as this can cause the wound to reopen or introduce bacteria, leading to infection.
9. Can I shower or swim with a laceration?
You should avoid swimming until the wound has fully healed and stitches (if applicable) have been removed. Depending on the severity of the laceration, your doctor may allow you to shower, but it’s important to keep the wound clean and dry. Waterproof bandages can help protect the wound while washing.
10. How do I know if my laceration is infected?
Signs of infection include increased redness, warmth, swelling, or pus drainage around the wound, as well as a foul smell. Fever or worsening pain may also indicate infection. If you suspect infection, seek medical attention immediately for proper treatment.