Wounds are disruptions in the continuity of tissue caused by trauma or injury, and they can vary widely in type and severity, including punctures, abrasions, lacerations, and contusions. The healing process of wounds is a complex and dynamic sequence of events involving multiple cellular mechanisms and phases such as hemostasis, inflammation, proliferation, and remodeling. Chronic wounds, which fail to heal within a typical timeframe, pose significant public health challenges due to their high prevalence and the substantial resources required for their management. Factors such as diabetes, aging, infection, and poor nutrition can impair the healing process, leading to chronic, non-healing wounds that cause considerable patient discomfort and economic burden. Understanding the cellular and molecular mechanisms underlying wound healing is crucial for developing effective therapies and improving patient outcomes.
Difference between acute and chronic wounds
Acute and chronic wounds differ significantly in their etiology, healing processes, and clinical management. Acute wounds typically result from external trauma or surgical procedures and follow a predictable healing process involving inflammation, tissue formation, and remodeling, often resolving within a few weeks. In contrast, chronic wounds, such as venous leg ulcers or diabetic foot ulcers, fail to progress through the normal stages of healing and persist for extended periods, often due to underlying conditions like chronic venous insufficiency or diabetes. Chronic wounds are characterized by persistent inflammation, high levels of pro-inflammatory cytokines, and the presence of bacterial biofilms, which impede healing and contribute to their recalcitrant nature. The management of chronic wounds is more complex, requiring a multidisciplinary approach and often involving advanced therapeutic strategies to address the underlying causes and promote healing. Recognizing these differences is crucial for effective wound care and the appropriate use of treatments, including antibiotics, to prevent complications such as antibiotic resistance.
Factors that contribute to wound formation
Wound formation is a complex process influenced by various factors that can impede the body’s natural healing mechanisms. Understanding these factors is crucial for effective prevention and treatment. Below are some key contributors to wound formation:
1. Poor Circulation/Oxygenation
Poor circulation and oxygenation significantly impair wound healing by reducing the supply of essential nutrients and oxygen to the wound site. This can lead to prolonged inflammation and delayed tissue repair. Hypoxia, or low oxygen levels, can hinder the function of immune cells and fibroblasts, which are crucial for wound closure and tissue regeneration. Additionally, poor circulation can exacerbate conditions like diabetes and cardiovascular diseases, further complicating the healing process.
2. Diabetes
Diabetes is a major factor contributing to impaired wound healing due to high blood glucose levels, poor circulation, and neuropathy. These conditions lead to reduced oxygenation and nutrient supply to the wound site, impairing the immune response and increasing the risk of infection. Diabetic patients often experience chronic wounds, such as diabetic foot ulcers, which are difficult to treat and can lead to severe complications like amputation if not managed properly.
3. Pressure/Mechanical Forces
Pressure and mechanical forces can cause tissue damage and impede wound healing by disrupting blood flow and causing ischemia. This is particularly evident in pressure ulcers, where prolonged pressure on the skin leads to tissue necrosis. Mechanical forces can also exacerbate inflammation and delay the healing process by continuously damaging the wound site, making it difficult for the body to repair the tissue effectively.
4. Age
Aging affects wound healing by altering the skin’s structure and function. Older individuals have thinner, less elastic skin with reduced collagen production, which impairs the wound healing process. Additionally, aging is associated with a decline in immune function and increased cellular senescence, leading to delayed wound closure and a higher risk of chronic wounds. These age-related changes make older adults more susceptible to infections and prolonged healing times.
5. Nutritional Deficiencies
Nutritional deficiencies can severely impact wound healing by depriving the body of essential nutrients required for tissue repair. Proteins, vitamins, and minerals play crucial roles in collagen synthesis, immune function, and cellular proliferation. Deficiencies in these nutrients can lead to delayed wound closure, increased infection risk, and impaired immune response, making it difficult for the body to heal wounds effectively.
6. Obesity
Obesity contributes to impaired wound healing through several mechanisms, including increased inflammation, poor circulation, and insulin resistance. Excess adipose tissue can lead to reduced blood flow and oxygenation to the wound site, while chronic inflammation associated with obesity can delay the healing process. Additionally, obesity is often linked with other conditions like diabetes, which further complicate wound healing.
7. Weakened Immune System
A weakened immune system can significantly impair wound healing by reducing the body’s ability to fight infections and clear debris from the wound site. Conditions such as diabetes, aging, and chronic diseases can weaken the immune response, leading to prolonged inflammation and delayed tissue repair. This makes individuals with compromised immune systems more susceptible to chronic wounds and infections.
8. Chronic Conditions
Chronic conditions such as cardiovascular disease, cancer, and diabetes can impede wound healing by affecting blood flow, immune function, and cellular processes. These conditions often lead to prolonged inflammation, reduced oxygenation, and impaired tissue regeneration, making it difficult for the body to heal wounds effectively. Chronic wounds associated with these conditions are challenging to treat and require specialized care.
9. Medications
Certain medications can interfere with wound healing by affecting immune function, blood clotting, and cellular proliferation. For example, corticosteroids and immunosuppressants can reduce inflammation but also impair the immune response, increasing the risk of infection. Anticoagulants can affect blood clotting, leading to prolonged bleeding and delayed wound closure. Understanding the impact of medications on wound healing is crucial for effective treatment.
10. Dry or Overly Moist Skin
The moisture balance of the skin is critical for optimal wound healing. Dry skin can lead to cracks and fissures, providing entry points for bacteria and increasing the risk of infection. Conversely, overly moist skin can cause maceration, weakening the skin’s integrity and making it more susceptible to damage. Maintaining an appropriate moisture level is essential for protecting the wound site and promoting efficient healing.
Types of Wounds
Wounds can be classified into various types based on their characteristics and healing processes. Understanding these classifications helps in determining the appropriate treatment and care. Below are some common types of wounds:
1. Acute Wounds
Acute wounds are injuries to the skin that occur suddenly and heal at a predictable and expected rate. These wounds typically progress through the normal stages of healing—hemostasis, inflammation, proliferation, and remodeling—without complications. Examples of acute wounds include cuts, scrapes, and surgical wounds. These types of wounds generally heal within a few weeks and do not require extensive medical intervention unless they become infected or are particularly deep.
2. Chronic Wounds
Chronic wounds are defined as wounds that fail to proceed through the normal stages of healing and remain in a prolonged inflammatory state. These wounds often persist for more than three months and are commonly associated with underlying conditions such as diabetes, vascular diseases, or prolonged pressure. Examples include diabetic foot ulcers, venous leg ulcers, and pressure ulcers. Chronic wounds pose significant challenges to healthcare providers due to their complex pathophysiology and the need for specialized treatment strategies.
3. Open vs. Closed Wounds
Open wounds are characterized by a break in the skin that exposes underlying tissues, making them susceptible to infection. Examples include abrasions, lacerations, and puncture wounds. Closed wounds, on the other hand, do not break the skin but may cause damage to underlying tissues, such as bruises or hematomas. Open wounds require careful cleaning and dressing to prevent infection, while closed wounds often need monitoring for internal damage and may require ice or compression to reduce swelling.
4. Simple vs. Complex Wounds
Simple wounds are those that involve minimal tissue damage and can be managed with basic wound care techniques, such as cleaning and dressing. Examples include minor cuts and abrasions. Complex wounds, however, involve significant tissue loss or damage and often require advanced medical interventions, such as surgical debridement, grafts, or specialized dressings. Complex wounds can be either acute or chronic and are often associated with conditions like diabetes or vascular diseases, making their management more challenging.
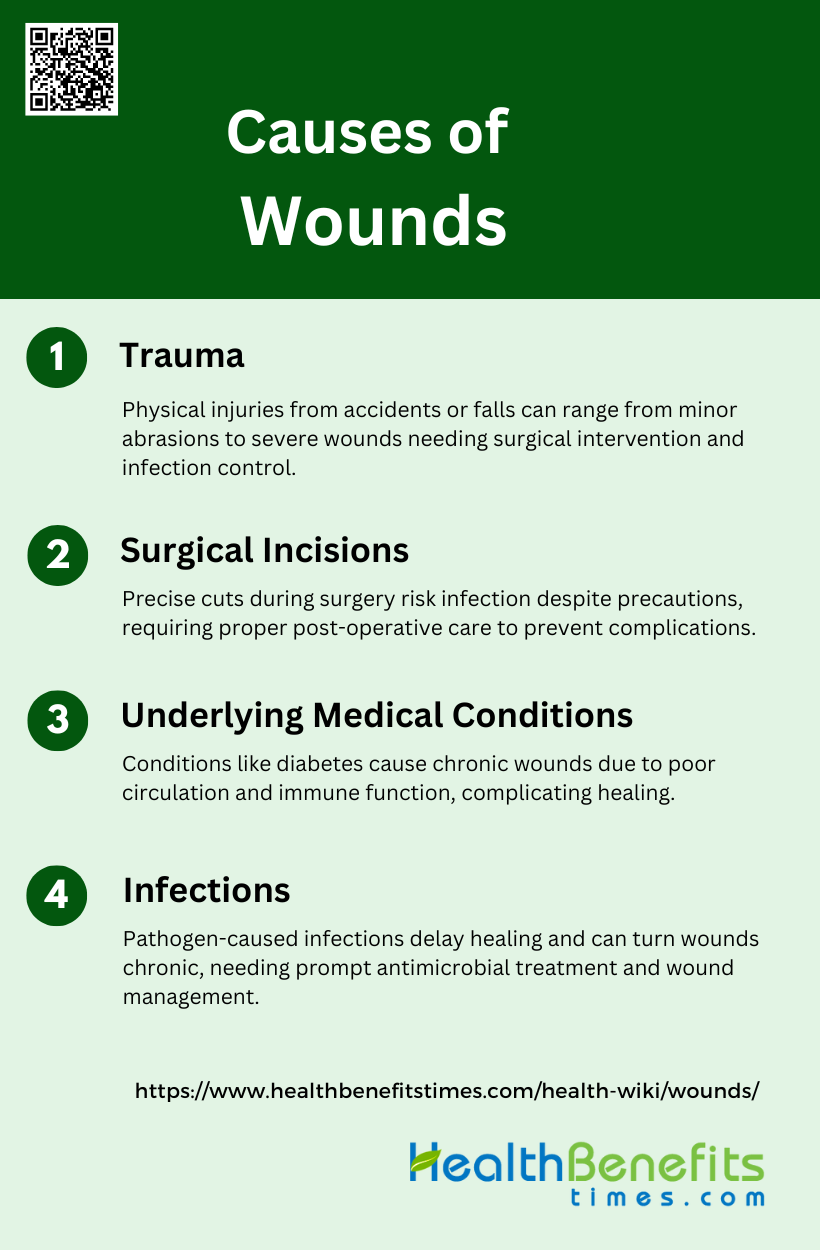
Causes of Wounds
Wounds can arise from a multitude of factors, each contributing to the disruption of skin integrity and tissue damage. Identifying these causes is essential for effective prevention and treatment. Below are some common causes of wounds:
1. Trauma
Traumatic wounds are caused by various forms of physical injury, including accidents, falls, and other injuries. These wounds can range from minor abrasions and lacerations to severe injuries involving extensive tissue damage, broken bones, and damage to internal organs. The management of traumatic wounds often involves the use of negative pressure wound therapy (NPWT), which aims to support wound healing, reduce infection risk, and prepare wounds for further surgical intervention. The risk of wound infection in trauma patients can be significant, with infection rates varying based on the level of bacterial contamination and the time from injury to surgical treatment. Effective management and timely intervention are crucial to prevent complications and promote healing.
2. Surgical Incisions
Surgical incisions are precise cuts made during surgical procedures, typically in a controlled environment with aseptic techniques to minimize infection risk. Despite these precautions, surgical site infections (SSIs) can still occur, particularly in cases of major trauma where the risk of infection can be as high as 27%. The type of dressing applied post-surgery, such as incisional negative-pressure wound therapy, can influence the infection rate and overall healing process. Proper post-operative care, including monitoring for signs of infection and ensuring appropriate wound management, is essential to reduce complications and support recovery.
3. Underlying Medical Conditions
Certain underlying medical conditions, such as diabetes and vascular diseases, can significantly impact wound healing. For instance, diabetic foot ulcers and venous leg ulcers are common chronic wounds associated with these conditions. These wounds often remain in the inflammatory stage and fail to progress to healing due to factors like poor circulation and high blood sugar levels. The presence of pathogenic bacteria and the formation of biofilms further complicate the healing process, making these wounds more resistant to treatment and prone to chronicity. Effective management requires addressing the underlying medical conditions and implementing targeted wound care strategies.
4. Infections
Infections are a major cause of wound complications and can be caused by bacterial, viral, or fungal pathogens. Bacterial infections are particularly common and can lead to chronic wounds if not properly managed. The presence of multiple bacterial species and the formation of biofilms can delay healing and increase resistance to antibiotics. War wounds, for example, are highly susceptible to infection due to the extensive tissue damage and contamination with environmental bacteria. Early and appropriate antimicrobial therapy, combined with surgical debridement and other interventions, is critical to prevent the development of severe infections and promote wound healing.
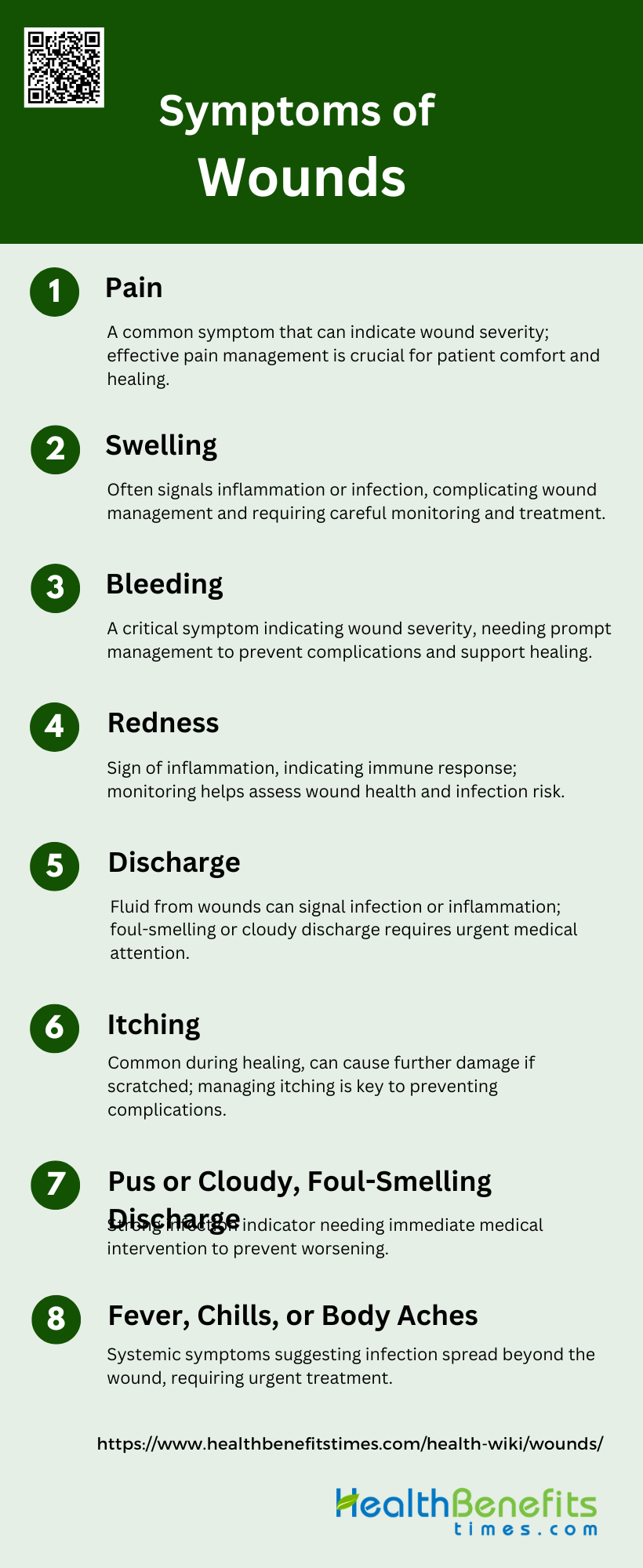
Symptoms of Wounds
Recognizing the symptoms of wounds is crucial for timely intervention and effective treatment. These symptoms can vary depending on the type and severity of the wound. Below are some common symptoms of wounds:
1. Pain
Pain is a common symptom associated with various types of wounds, including malignant fungating wounds and infected diabetic wounds. Patients often report significant discomfort, which can be exacerbated by the presence of other symptoms such as swelling and discharge. Pain management is crucial in wound care, as it directly impacts the patient’s quality of life and functional performance. For instance, the Toronto Symptom Assessment System for Wounds (TSAS-W) identifies pain as one of the most prevalent symptoms, necessitating effective pain management strategies to alleviate patient distress.
2. Swelling
Swelling is another frequent symptom observed in wound conditions, often indicating an inflammatory response. It is commonly seen in infected wounds, where it is accompanied by other signs of infection such as redness and increased local temperature. Swelling can complicate wound management by causing additional pain and limiting mobility. In the context of skeletal external fixator pin sites, significant differences in swelling were noted between calm, irritated, and infected states, highlighting its role as a key indicator of wound status.
3. Bleeding
Bleeding is a critical symptom that can occur in various wound types, including malignant fungating wounds and traumatic injuries. It is often associated with the severity of the wound and can complicate the healing process. In malignant wounds, bleeding is one of the multiple symptoms that patients experience, contributing to the overall symptomatic burden. Effective management of bleeding is essential to prevent further complications and to promote wound healing.
4. Redness
Redness is a classic sign of inflammation and is commonly observed in both acute and chronic wounds. It indicates increased blood flow to the affected area as part of the body’s immune response. Redness is often accompanied by other symptoms such as heat, swelling, and pain. In the context of wound care, redness can help differentiate between various states of wound health, such as calm, irritated, and infected pin sites.
5. Discharge
Discharge from a wound can vary in appearance and consistency, ranging from clear fluid to pus. It is often a sign of infection or inflammation and can indicate the severity of the wound. The presence of discharge, especially if it is foul-smelling or cloudy, necessitates prompt medical attention to prevent further complications. The TSAS-W identifies exudation as a prevalent symptom, emphasizing the need for effective wound management strategies to control discharge.
6. Itching
Itching is a common symptom in wound healing, often associated with the inflammatory response. It can be particularly distressing for patients, leading to scratching and potential further damage to the wound site. In the case of malignant fungating wounds, pruritus (itching) is one of the multiple symptoms that patients report, affecting their overall comfort and quality of life. Effective management of itching is essential to prevent secondary infections and promote healing.
7. Pus or Cloudy, Foul-Smelling Discharge
The presence of pus or a cloudy, foul-smelling discharge is a strong indicator of infection in a wound. This symptom necessitates immediate medical intervention to prevent the spread of infection and further complications. Infected diabetic wounds, for example, often present with yellowish pus discharge, highlighting the need for effective antimicrobial treatment. The presence of such discharge is a critical factor in diagnosing and managing wound infections.
8. Fever, Chills, or Body Aches
Fever, chills, and body aches are systemic symptoms that can accompany severe wound infections. These symptoms indicate that the infection may have spread beyond the local wound site, requiring urgent medical attention. In the context of wound care, the presence of fever and other systemic symptoms can help differentiate between localized and systemic infections, guiding appropriate treatment strategies. For instance, patients with infected pin sites often report feeling unwell or feverish, underscoring the need for comprehensive infection management.
Diagnosing Wounds
Accurate diagnosis of wounds is essential for effective treatment and recovery. This process involves a series of steps to thoroughly assess the wound and the patient’s overall health. The following sections outline the key components of wound diagnosis:
1. Physical Examination
A thorough physical examination is crucial for diagnosing wounds accurately. This involves a detailed visual and manipulative assessment to understand the extent and nature of the wound. For instance, in equine limb wounds, a complete physical examination helps in identifying the systemic and local tissue influences, which is essential for effective treatment. Similarly, in cases of penetrating extremity trauma, physical examination, including the assessment of “hard signs” of vascular injury, is vital for timely and accurate diagnosis to prevent significant morbidity. Additionally, in forensic pathology, physical examination combined with advanced diagnostic techniques like radiological and MRI examinations can provide a detailed understanding of the wound.
2. Medical History Review
Reviewing the medical history of a patient is a fundamental step in wound diagnosis. This includes gathering information on the duration of the wound, previous ulcerations, trauma history, and underlying medical conditions such as diabetes or peripheral vascular disease. For instance, in wound care, a comprehensive history helps in identifying systemic factors that may affect wound healing, such as arterial or venous insufficiency, and previous injuries. In chronic wounds, understanding the patient’s medical background, including family history and previous treatments, is essential for developing an effective management plan. This detailed history aids in forming a diagnostic hypothesis before initiating treatment.
3. Imaging and Tests
Imaging and diagnostic tests play a critical role in assessing the extent and nature of wounds. Techniques such as plain radiography, computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound are valuable for diagnosing deeper wound infections and determining the involvement of underlying structures. For example, in the diagnosis of arterial injury in penetrating extremity trauma, ultrasonography and Ankle-Brachial Index (ABI) are used to evaluate the need for further interventions like CT angiography. Additionally, in forensic wound examination, advanced imaging techniques and molecular biological methods, such as cytokine analysis, help in determining the age and vitality of wounds. These diagnostic tools provide a comprehensive understanding of the wound, aiding in accurate diagnosis and effective treatment planning.
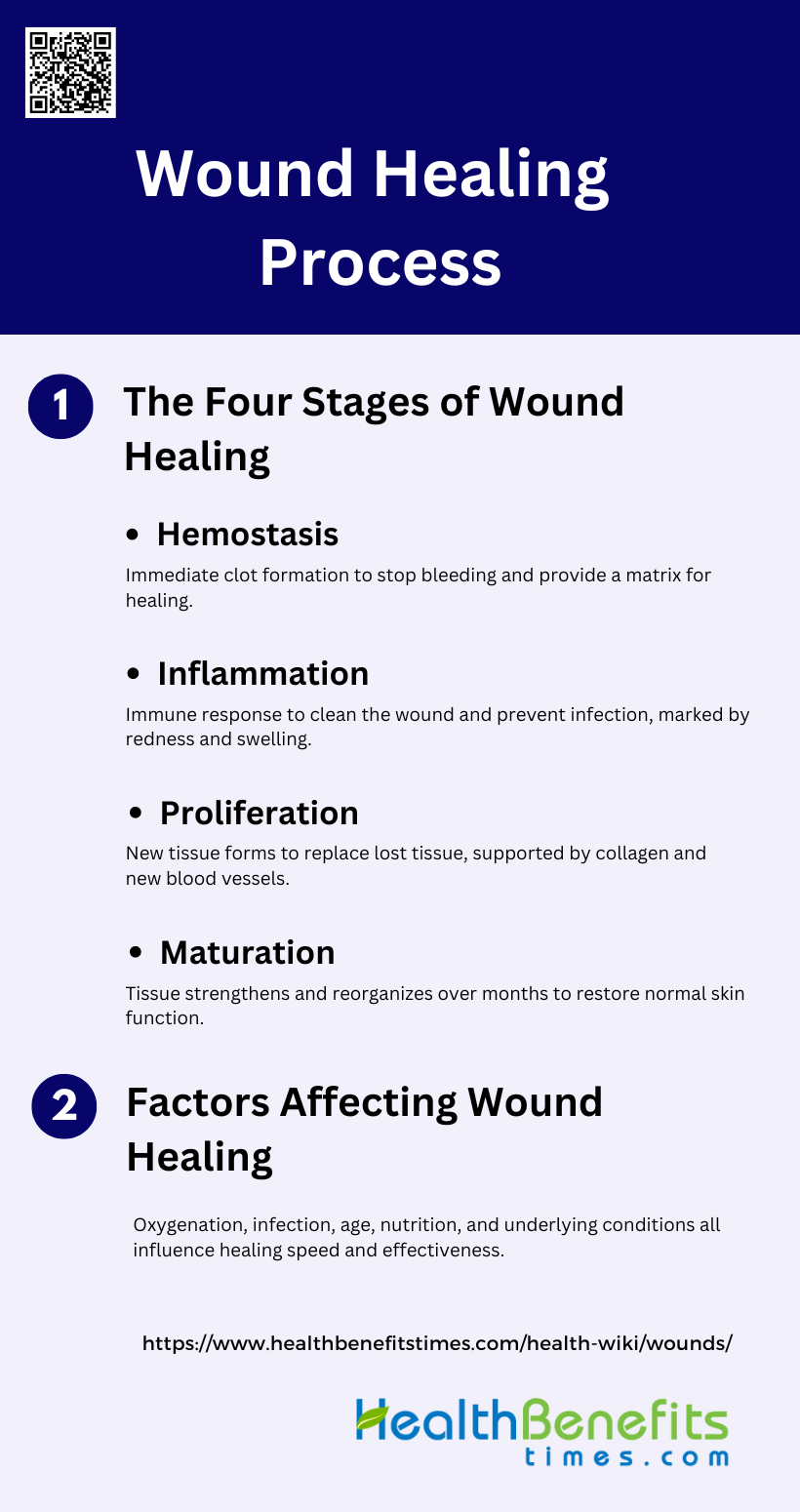
Wound Healing Process
Understanding the wound healing process is essential for effective treatment and recovery. This process involves several stages and is influenced by various factors. The following sections detail the stages of wound healing and the factors that can affect it:
1. The Four Stages of Wound Healing
1. Hemostasis: Hemostasis is the immediate response to injury, aiming to stop bleeding. When tissue is injured, blood components spill into the site, and platelets come into contact with exposed collagen and other elements of the extracellular matrix. This contact triggers the release of clotting factors and essential growth factors such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-beta), which are crucial for initiating the wound healing process. The formation of a blood clot not only stops bleeding but also provides a temporary matrix for incoming cells.
2. Inflammation: The inflammation phase is the body’s response to injury and prevention of infection. Neutrophils are the first to arrive at the wound site, performing phagocytosis to remove foreign materials, bacteria, and damaged tissue. Macrophages follow, continuing the process of phagocytosis and releasing more PDGF and TGF-beta to further the healing process. This phase is characterized by redness, heat, swelling, and pain, which are signs of the body’s immune response working to clean the wound and prevent infection.
3. Proliferation: During the proliferation phase, new tissue forms to replace what was lost. Fibroblasts migrate to the wound site to deposit new extracellular matrix, primarily collagen, which provides structural support. This phase also involves reepithelialization, angiogenesis, and peripheral nerve repair. The new tissue gradually fills the wound, and the formation of new blood vessels ensures an adequate supply of nutrients and oxygen, which are essential for tissue repair and regeneration.
Maturation: The maturation phase, also known as remodeling, involves the strengthening and reorganization of the newly formed tissue. Collagen fibers are realigned, and the extracellular matrix is remodeled to increase the tensile strength of the wound site. This phase can last for months to years, during which the wound gradually regains its normal function and appearance. The goal is to restore the skin’s integrity and functionality as closely as possible to its pre-injury state.
2. Factors Affecting Wound Healing
Wound healing can be influenced by various factors, including oxygenation, infection, age, sex hormones, stress, diabetes, obesity, medications, alcoholism, smoking, and nutrition. Oxygenation is crucial as it supports cellular functions and energy production necessary for healing. Infection can delay healing by prolonging the inflammatory phase and causing additional tissue damage. Age and sex hormones also play roles, with older age and hormonal imbalances potentially slowing the healing process. Stress, diabetes, and obesity can impair immune function and reduce blood flow, further complicating wound repair. Medications, alcoholism, and smoking can negatively impact cellular activities and blood circulation, while proper nutrition provides the essential building blocks for tissue repair. Understanding these factors can lead to better therapeutic strategies to improve wound healing outcomes.
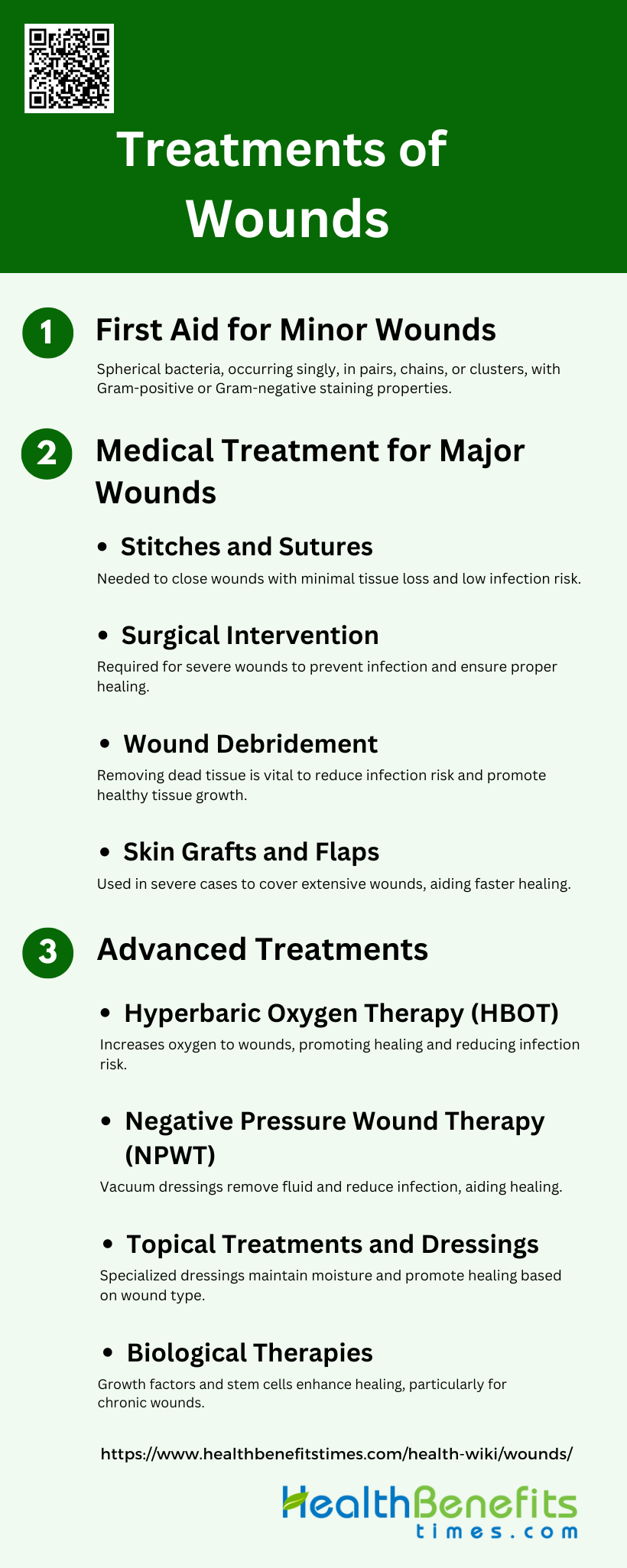
Treatments of Wounds
Effective wound treatment varies based on the severity and type of the wound. From basic first aid to advanced medical interventions, each method aims to promote healing and prevent complications. The following sections outline the different treatments for minor, major, and complex wounds:
A. First Aid for Minor Wounds
1. Cleaning and Dressing Small Wounds: Cleaning small wounds with antiseptics and dressing them properly can prevent infection and promote healing. Using antiseptics like iodine or zinc oxide mesh dressings can help, although evidence on their effectiveness is mixed.
2. Over-the-Counter Antibiotic Ointments and Pain Relief: Topical antibiotic ointments, such as sucralfate cream, can increase the likelihood of healing and reduce pain in minor wounds compared to standard treatments.
B. Medical Treatment for Major Wounds
1. Stitches and Sutures: When and Why They Are Needed: Stitches, staples, adhesives, or clips are used to close surgical incisions, promoting healing by primary intention. This method is typically used when the risk of infection is low and tissue loss is minimal.
2. Surgical Intervention: For Severe Cases: Severe wounds, such as deep lacerations or avulsions, may require surgical intervention to close the wound and prevent infection. This is crucial when there is significant tissue loss or high infection risk.
3. Wound Debridement: Removing Dead Tissue to Promote Healing: Debridement, the removal of dead tissue, is essential for promoting healing in major wounds. This process helps to reduce infection risk and allows healthy tissue to grow.
4. Skin Grafts and Flaps: Used in Severe Cases: In cases of severe burns or large avulsions, skin grafts and flaps are used to cover extensive wounds, promoting faster and more effective healing.
C. Advanced Treatments
1. Hyperbaric Oxygen Therapy (HBOT): HBOT increases oxygen supply to the wound area, promoting faster healing and reducing infection risk. This therapy is particularly useful for chronic and non-healing wounds.
2. Negative Pressure Wound Therapy (NPWT): NPWT uses vacuum dressings to promote healing by removing excess fluid and reducing infection risk. However, evidence on its effectiveness for surgical wounds healing by secondary intention is limited and inconclusive.
3. Topical Treatments and Dressings: Various dressings, such as hydrocolloids, alginates, and foams, are used depending on the wound type. These dressings help maintain a moist environment, which is conducive to healing.
4. Biological Therapies: Biological agents, including growth factors and stem cells, are used to enhance the healing process. These therapies can be particularly effective in treating chronic and non-healing wounds.
Complications of Untreated Wounds
Leaving wounds untreated can lead to serious health issues and complications. Understanding these potential risks is crucial for timely and effective wound management. The following sections detail the various complications that can arise from untreated wounds:
1. Infections and Abscesses
Untreated wounds are highly susceptible to infections, which can significantly complicate the healing process. Bacterial colonization at the wound site can lead to the formation of biofilms, which are communities of bacteria that adhere to the wound surface and are resistant to antibiotics. These biofilms contribute to persistent inflammation and delay healing, often resulting in chronic wound conditions such as diabetic foot ulcers, venous leg ulcers, and pressure ulcers. In severe cases, infections can progress to systemic infections, sepsis, and multiple organ dysfunction syndrome, posing life-threatening risks.
2. Delayed Healing
Delayed healing is a common complication of untreated wounds, often resulting from sustained inflammation and the presence of biofilms. Chronic wounds, which fail to progress through the normal stages of healing, remain in the inflammatory phase due to various factors, including bacterial colonization and immune system dysregulation. This prolonged inflammatory response can be exacerbated by underlying conditions such as diabetes, cardiovascular disease, and aging, which further impede the healing process. Effective wound management strategies are essential to overcome these barriers and promote timely healing.
3. Scarring and Tissue Damage
Untreated wounds can lead to significant scarring and tissue damage, which may result in functional and aesthetic impairments. The prolonged inflammatory phase and the presence of biofilms in chronic wounds contribute to excessive tissue degradation and impaired tissue regeneration. This imbalance between tissue synthesis and degradation can result in misshapen scars and compromised tissue integrity. Proper wound care, including debridement, infection control, and the use of advanced therapies, is crucial to minimize scarring and promote optimal tissue repair.
4. Chronic Wound Development
Chronic wounds are a severe complication of untreated wounds, characterized by their failure to heal within a typical timeframe. These wounds remain in a state of chronic inflammation, often due to persistent bacterial infections and biofilm formation. Chronic wounds, such as diabetic foot ulcers, venous leg ulcers, and pressure ulcers, pose significant challenges to healthcare systems due to their high prevalence and the complexity of their management. Understanding the underlying pathophysiology and implementing comprehensive wound care strategies are essential to prevent the development of chronic wounds and improve patient outcomes.
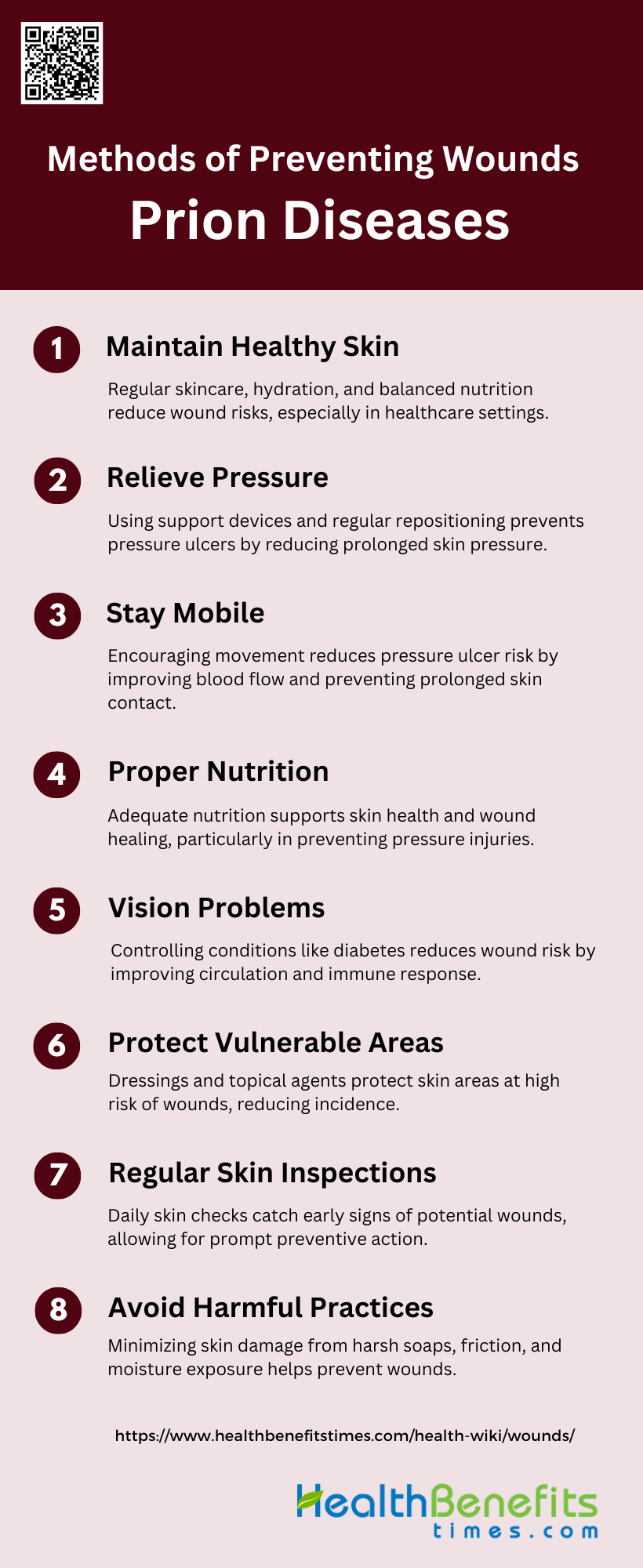
Methods of Preventing Wounds
Preventing wounds is essential for maintaining overall health and well-being. By adopting certain practices and making lifestyle changes, the risk of developing wounds can be significantly reduced. The following sections outline various methods to prevent wounds:
1. Maintain Healthy Skin
Maintaining healthy skin is crucial in preventing wounds, particularly in healthcare settings. A comprehensive skin care regimen that includes proper hydration, balanced nutrition, and the use of moisturizers can significantly reduce the incidence of skin tears and pressure ulcers. Studies emphasize the importance of starting these regimens immediately upon a patient’s arrival in institutions such as hospitals or residential aged care facilities and continuing them throughout their stay. Ensuring the skin’s pH balance and addressing issues like dry or friable skin are also key components of maintaining skin health.
2. Relieve Pressure
Relieving pressure on vulnerable areas of the body is essential to prevent pressure ulcers, which are localized injuries to the skin and underlying tissue. Strategies include the use of support mattresses, cushions, and regular repositioning schedules. Research indicates that silicone dressings may reduce the incidence of pressure ulcers, although the evidence is of low certainty and further studies are needed. Repositioning patients at regular intervals, such as every two to four hours, can also help in redistributing pressure and preventing skin breakdown.
3. Stay Mobile
Encouraging mobility is a key strategy in wound prevention. Patients who are able to move and reposition themselves are less likely to develop pressure ulcers. Mobility training and strengthening exercises can significantly contribute to the successful prevention and treatment of wounds. Regular movement helps in maintaining blood flow and reducing prolonged pressure on any one part of the body, thereby minimizing the risk of skin breakdown and ulcer formation.
4. Proper Nutrition
Proper nutrition plays a pivotal role in wound prevention and healing. Adequate intake of macronutrients and micronutrients is necessary to maintain and repair body tissues. Nutritional support, including the use of protein supplements and ensuring a balanced diet, is recommended to prevent pressure injuries. Specific nutrients like arginine have been shown to promote wound healing, especially in older adults in acute and long-term care settings. Ensuring patients receive sufficient nutrition can significantly impact their overall skin health and ability to recover from wounds.
5. Manage Underlying Health Conditions
Managing underlying health conditions such as diabetes, vascular diseases, and immobility is crucial in preventing wounds. These conditions can impair blood flow and skin integrity, making patients more susceptible to pressure ulcers and other types of wounds. Regular monitoring and treatment of these conditions, along with patient education on managing their health, can help in reducing the risk of wound development. Effective management of these conditions involves a multidisciplinary approach, including medical, nutritional, and physical therapy interventions.
6. Protect Vulnerable Areas
Protecting vulnerable areas of the body, such as bony prominences, is essential in wound prevention. The use of dressings and topical agents can provide a protective barrier and reduce the risk of skin breakdown. Studies have shown that fatty acid-containing treatments and silicone dressings may help in reducing the incidence of pressure ulcers, although the evidence is not conclusive and further research is needed. Regular inspection and appropriate use of protective devices can help in safeguarding these areas from injury.
7. Regular Skin Inspections
Regular skin inspections are a fundamental part of wound prevention. Daily checks can help in early identification of potential problem areas, allowing for timely intervention. This practice is particularly important for patients at high risk of developing pressure ulcers, such as those with limited mobility or incontinence. Inspections should include looking for signs of redness, swelling, or other changes in skin condition. Early detection and treatment can prevent minor issues from developing into more serious wounds.
8. Avoid Harmful Practices
Avoiding harmful practices that can damage the skin is crucial in wound prevention. This includes minimizing the use of harsh soaps, avoiding excessive friction and shear, and ensuring that patients are not exposed to prolonged moisture from incontinence or sweating. Gentle cleaning and the use of appropriate skin care products can help in maintaining skin integrity. Educating patients and caregivers on proper skin care techniques and the importance of avoiding harmful practices can significantly reduce the risk of wound development.
When to Seek Medical Attention
Signs that a wound requires professional medical care
A wound may necessitate professional medical attention if it exhibits excessive bleeding, signs of infection, or contains foreign objects. Excessive bleeding that does not stop after applying pressure for several minutes can indicate a deeper injury that needs medical intervention. Signs of infection, such as redness, swelling, warmth, and pus, suggest that the body’s natural defenses are overwhelmed and require antibiotics or other treatments to prevent further complications. Additionally, foreign objects embedded in the wound can introduce bacteria and other pathogens, making it crucial to seek medical help to properly clean and close the wound.
Risks of untreated or improperly treated wounds
Untreated or improperly treated wounds pose significant risks, including infections, delayed healing, and the development of chronic wounds. Infections can lead to severe complications such as cellulitis, abscess formation, and even systemic infections like sepsis if not promptly addressed. Delayed healing can result from factors like hypoxia, persistent infection, or the presence of foreign bodies, which can prolong the inflammatory phase and prevent the wound from progressing to the proliferative and maturation phases. Chronic wounds, such as diabetic foot ulcers and pressure ulcers, can develop when wounds fail to heal within a typical timeframe, leading to prolonged discomfort, increased healthcare costs, and a higher risk of further complications.
FAQs
1. How do environmental factors influence wound healing?
Environmental factors like temperature, humidity, and air quality can impact wound healing. For example, a warm and moist environment typically promotes faster healing, while extreme temperatures or dry conditions can delay the process. Additionally, exposure to pollutants and allergens can increase the risk of wound infection.
2. What role does mental health play in wound healing?
Mental health can significantly affect wound healing. Stress, anxiety, and depression can impair the immune system and slow down the healing process. Managing mental health through relaxation techniques, therapy, and stress-reduction strategies can support better wound outcomes.
3. Can alternative therapies like herbal treatments aid in wound healing?
Certain herbal treatments, such as calendula, honey, and aloe vera, have been shown to promote wound healing by reducing inflammation, providing antimicrobial effects, and supporting tissue regeneration. However, their efficacy varies, and they should be used alongside, not in place of, conventional treatments.
4. How does hydration affect wound healing?
Proper hydration is essential for maintaining skin elasticity and supporting cellular functions involved in wound repair. Dehydration can lead to dry, brittle skin, which is more prone to injury and slower to heal. Drinking sufficient water and maintaining balanced electrolytes are important for optimal wound healing.
5. What are the potential complications of using traditional dressings vs. advanced dressings?
Traditional dressings, such as gauze, may sometimes stick to the wound and disrupt healing when removed. Advanced dressings, like hydrocolloids or alginates, maintain a moist environment that can accelerate healing and reduce pain during dressing changes. However, advanced dressings may be more expensive and require more careful monitoring.
6. How does wound healing differ between various age groups?
Wound healing is typically faster in younger individuals due to more robust cellular regeneration and immune response. In older adults, the healing process is often slower because of thinner skin, reduced collagen production, and a weaker immune system, which increases the risk of complications.
7. Are there specific diets that can enhance wound healing?
A diet rich in proteins, vitamins (such as vitamin C and vitamin A), minerals (like zinc and iron), and antioxidants can enhance wound healing by supporting tissue repair, reducing inflammation, and strengthening the immune system. Certain amino acids, like arginine and glutamine, are also beneficial.
8. Can wounds heal without scarring, and how can scarring be minimized?
While some wounds can heal with minimal scarring, the extent of scarring often depends on the wound’s depth, location, and the individual’s skin type. Techniques to minimize scarring include keeping the wound moist, using silicone gel sheets, massaging the scar tissue, and in some cases, using corticosteroid injections or laser therapy.
9. What is the role of genetics in wound healing?
Genetics can influence how quickly and effectively wounds heal. Some individuals may have a genetic predisposition to slower healing or excessive scarring, such as keloids. Understanding one’s genetic factors can help tailor personalized wound care strategies.
10. How does smoking affect wound healing?
Smoking significantly impairs wound healing by reducing blood flow, decreasing oxygen delivery to tissues, and impairing immune function. Nicotine constricts blood vessels, and carbon monoxide reduces the oxygen-carrying capacity of the blood, both of which delay the healing process.