An antiseptic is a substance that inhibits the growth and development of microorganisms on living tissues, particularly the skin. They are widely used in medical settings to prevent infections, especially during surgical procedures and in the treatment of wounds. Antiseptics work by being toxic to bacteria, aiding in their mechanical removal from the skin, and are crucial in reducing the risk of surgical site infections (SSIs). Common antiseptics include iodine, chlorhexidine, and alcohol-based solutions, each with varying degrees of effectiveness and application methods. Despite their widespread use, the effectiveness of different antiseptics can vary, and factors such as the type of antiseptic, its concentration, and the method of application play significant roles in their efficacy. Antiseptics are also used in chronic wound care to prevent infections and promote healing, especially in the context of increasing bacterial resistance to antibiotics.
Difference between antiseptics, disinfectants, and antibiotics
Antiseptics, disinfectants, and antibiotics are all antimicrobial agents, but they differ in their applications and mechanisms of action. Antiseptics are chemicals used on living tissues to reduce the risk of infection by killing or inhibiting the growth of microorganisms; common examples include alcohols, iodine, and chlorine compounds. Disinfectants, on the other hand, are used on non-living surfaces to destroy microorganisms and prevent their spread; they include agents like aldehydes, peroxygens, and phenolic compounds. Antibiotics are substances, often derived from microorganisms, that specifically target and kill or inhibit other microorganisms within the body, and they are typically used to treat bacterial infections. While antiseptics and disinfectants can have broad-spectrum antimicrobial activity, antibiotics are more specific and can lead to bacterial resistance if misused.
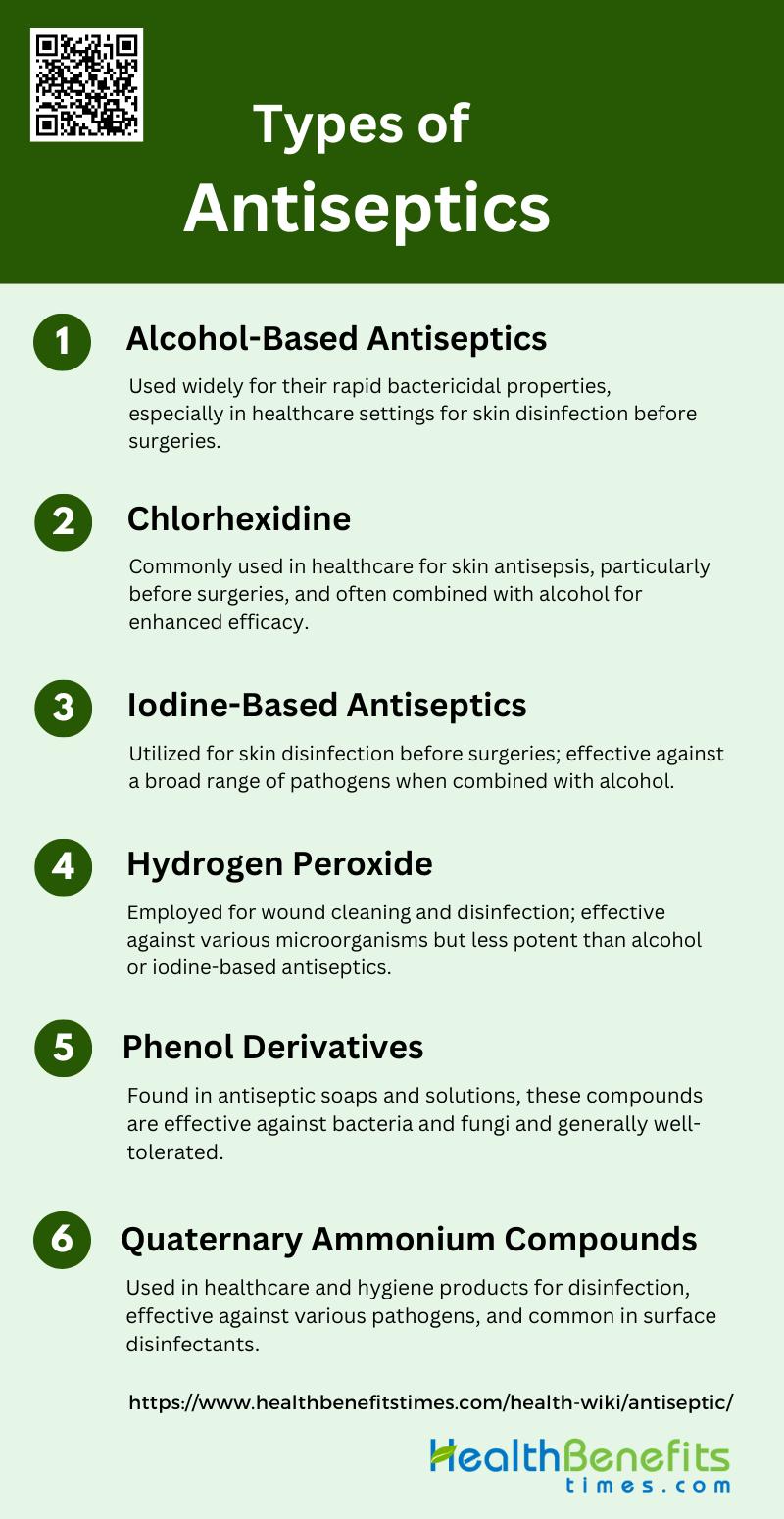
Types of Antiseptics
Antiseptics play a vital role in infection control by eliminating or inhibiting the growth of harmful microorganisms on living tissues. They are commonly used in medical settings, personal hygiene, and wound care. Below are various types of antiseptics:
1. Alcohol-Based Antiseptics
Alcohol-based antiseptics, such as isopropyl alcohol and ethanol, are widely used for their rapid bactericidal and fungicidal properties. They are effective in various healthcare settings for skin disinfection before procedures and surgeries. Isopropyl alcohol (70% v/v) has shown significant efficacy against a broad spectrum of bacteria and fungi. These antiseptics are often combined with other agents like chlorhexidine to enhance their effectiveness.
2. Chlorhexidine
Chlorhexidine is commonly used in healthcare settings for skin antisepsis, particularly before surgeries and catheter insertions. It is often combined with alcohol to improve its efficacy. Studies have shown that chlorhexidine-alcohol solutions are more effective than povidone-iodine-alcohol in reducing surgical wound contamination and catheter-related infections. However, chlorhexidine can cause severe skin reactions in some patients.
3. Iodine-Based Antiseptics
Iodine-based antiseptics, including povidone-iodine and traditional tincture iodine, are used for skin disinfection before surgeries and in wound care. Povidone-iodine is effective against a wide range of pathogens and is often used in combination with alcohol for enhanced efficacy. Tincture of iodine (2%) has also demonstrated strong bactericidal and fungicidal activity.
4. Hydrogen Peroxide
Hydrogen peroxide is used as an antiseptic for wound cleaning and disinfection. It is effective against a variety of microorganisms but is less potent compared to alcohol-based and iodine-based antiseptics. Its efficacy can be influenced by contact time and organic load. Hydrogen peroxide is often used in situations where other antiseptics might cause irritation or allergic reactions.
5. Phenol Derivatives
Phenol derivatives, such as chloroxylenol, are used for their antimicrobial properties in various healthcare and household products. They are effective against a range of bacteria and fungi and are commonly found in antiseptic soaps and solutions. These compounds are generally well-tolerated and provide a broad spectrum of antimicrobial activity.
6. Quaternary Ammonium Compounds
Quaternary ammonium compounds are used in healthcare settings and personal hygiene products for their disinfectant properties. They are effective against a variety of pathogens and are often used in surface disinfectants and hand sanitizers. These compounds are valued for their ability to reduce microbial load on surfaces and skin.
Uses of Antiseptics
Antiseptics are essential for preventing infections by eliminating or inhibiting the growth of microorganisms. They are used in various settings, including healthcare, personal hygiene, first aid, and household cleaning. Below are some common uses of antiseptics in different contexts:
1. In Healthcare Settings
Antiseptics are crucial in healthcare settings for various applications. They are used for preoperative skin preparation to reduce the risk of surgical site infections (SSIs) by removing soil and transient organisms from the skin where a surgical incision will be made. Additionally, antiseptics are employed in basic hand hygiene, antiseptic bathing, and pre-surgical care with alcohol/chlorhexidine to reduce skin microflora and prevent infections. Despite their benefits, there is a risk of contamination with pathogenic organisms, which necessitates careful consideration of their use.
2. In Personal Hygiene
In personal hygiene, antiseptics are commonly found in hand sanitizers, mouthwashes, and antiseptic creams. Alcohol-based hand sanitizers are particularly effective for rapidly destroying pathogens on lightly soiled hands, making them a popular choice for hand disinfection in both healthcare and public settings. These products are convenient as they do not require water or hand drying materials, although their effectiveness can be compromised by heavy soil loads.
3. In First Aid
Antiseptics play a vital role in first aid by being applied to cuts, wounds, and insect bites to prevent infections. They help in cleaning the affected area and reducing the microbial load, thereby promoting faster healing and preventing complications. The use of antiseptics in first aid is a common practice due to their broad-spectrum antimicrobial activity, which is effective against a wide range of pathogens.
4. In Household Cleaning
In household cleaning, antiseptics are used to disinfect surfaces and prevent microbial growth. Products containing active chemical agents like alcohols, phenols, iodine, and chlorine are extensively used for cleaning hard surfaces to maintain hygiene and reduce the risk of infections. These agents are effective in killing a broad spectrum of microorganisms, making them essential for maintaining a clean and safe home environment.
Safety Considerations of Antiseptic
Ensuring the safe use of antiseptics involves understanding their potential side effects, following proper usage guidelines, and adhering to best practices for storage and handling. Below are key safety considerations of antiseptics.
1. Potential Side Effects
Antiseptics, while effective in reducing surgical site infections (SSIs), can cause several side effects, including allergic reactions and skin irritation. Chlorhexidine, a commonly used antiseptic, has been associated with skin burns and breakdown, particularly in neonatal intensive care units. Additionally, studies have reported mild adverse events such as erythema, pruritus, dermatitis, and mild allergic symptoms with various antiseptic agents. Despite these side effects, the frequency of severe adverse reactions remains low, and the benefits of using antiseptics often outweigh the risks.
2. Proper Usage Guidelines
Proper usage of antiseptics is crucial for their effectiveness in preventing SSIs. For instance, chlorhexidine in alcohol has been shown to significantly reduce the risk of SSIs compared to iodine-alcohol solutions. The application method and concentration of the antiseptic are also important; for example, 2.0-2.5% chlorhexidine in alcohol is recommended for its efficacy. It is essential to follow specific guidelines for antiseptic use, including allowing the solution to dry completely before making an incision to maximize its bactericidal effects. Adhering to these guidelines ensures the optimal performance of antiseptics in clinical settings.
3. Storage and Handling
Proper storage and handling of antiseptics are vital to maintain their efficacy and safety. Antiseptics should be stored in a cool, dry place away from direct sunlight to prevent degradation. Alcohol-based solutions, such as those containing chlorhexidine, should be handled with care due to their flammability, especially in hair-bearing areas. It is also important to use antiseptics within their expiration dates and to follow manufacturer instructions for storage conditions. Ensuring that antiseptics are stored and handled correctly helps maintain their effectiveness and reduces the risk of adverse reactions.
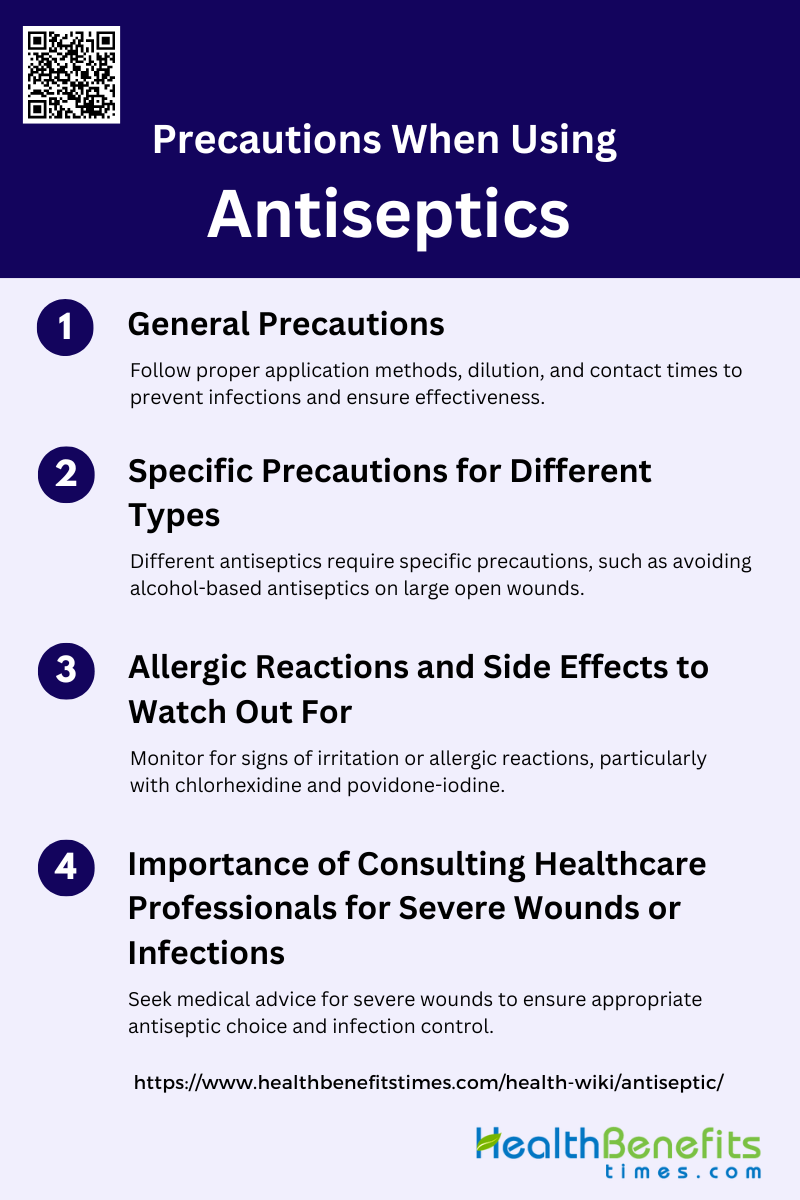
Precautions When Using Antiseptics
Using antiseptics safely requires awareness of potential risks and adherence to recommended guidelines. Proper application, storage, and handling are crucial to ensure their effectiveness and minimize adverse effects. Below are some important precautions to consider when using antiseptics.
1. General Precautions
When using antiseptics, it is crucial to follow correct application methods, ensure proper dilution, and maintain adequate contact time to maximize their effectiveness. Proper application helps in reducing the risk of surgical site infections (SSIs) by effectively removing soil and transient organisms from the skin. Additionally, ongoing staff education, monitoring, and feedback are essential to maintain optimal application protocols and prevent healthcare-associated infections.
2. Specific Precautions for Different Types
Different types of antiseptics require specific precautions. For instance, alcohol-based antiseptics should be avoided on large open wounds due to their potential to cause irritation and delay healing. Chlorhexidine gluconate (CHG) is preferred for skin preparation prior to central and arterial intravascular catheter insertions, while povidone-iodine (PVP-I) is effective for a broader spectrum of microorganisms but should be used cautiously due to potential side effects. It is also important to avoid using non-sterile antiseptics on mucous membranes to prevent infections.
3. Allergic Reactions and Side Effects to Watch Out For
Allergic reactions and side effects are important considerations when using antiseptics. Povidone-iodine (PVP-I) has been associated with adverse events, including skin irritation and allergic reactions, although it has low allergenic properties compared to other antiseptics. Chlorhexidine gluconate (CHG) can also cause skin irritation and allergic reactions in some individuals. Monitoring for signs of allergic reactions and side effects is crucial to ensure patient safety.
4. Importance of Consulting Healthcare Professionals for Severe Wounds or Infections
For severe wounds or infections, it is essential to consult healthcare professionals to determine the most appropriate antiseptic and treatment plan. Healthcare professionals can provide guidance on the best antiseptic to use based on the specific wound type and patient condition, ensuring effective infection control and promoting healing. They can also help in tailoring antiseptic regimens to avoid complications and optimize patient outcomes.
Common Misconceptions about Antiseptics
Antiseptics are widely used, but there are several misconceptions about their effectiveness and usage. Understanding the facts can help ensure they are used correctly and safely. Below are some common misconceptions about antiseptics and the truths behind them.
1. Antiseptics kill all microorganisms.
Antiseptics are effective against a broad spectrum of microorganisms, including bacteria, fungi, and viruses, but they do not kill all microorganisms. For example, while povidone-iodine (PVP-I) has a broad spectrum of antimicrobial activity, it is not effective against all types of microorganisms, and its efficacy can be influenced by factors such as the presence of organic matter. Additionally, the effectiveness of antiseptics can vary depending on the type and concentration used.
2. Antiseptics and disinfectants are the same thing.
Antiseptics and disinfectants are often confused, but they serve different purposes. Antiseptics are used on living tissues to reduce the risk of infection, while disinfectants are used on inanimate objects to kill microorganisms. The effectiveness and safety profiles of these substances differ significantly, with antiseptics being formulated to be less harsh on skin and tissues.
3. More antiseptic is always better.
Using more antiseptic does not necessarily lead to better outcomes and can sometimes be counterproductive. Overuse of antiseptics can lead to issues such as skin irritation, cytotoxicity, and the potential development of antimicrobial resistance. The effectiveness of antiseptics is also dependent on proper application methods rather than the quantity used.
4. Antiseptics never cause side effects.
Antiseptics can cause side effects, including skin irritation, allergic reactions, and cytotoxicity. For instance, while povidone-iodine is generally well-tolerated, it can still cause allergic reactions in some individuals. The choice of antiseptic should consider potential side effects and individual patient tolerability.
5. Antiseptics are always necessary for wound care.
While antiseptics can be beneficial in preventing and treating infections in wound care, they are not always necessary. The necessity of antiseptics depends on the type of wound, the risk of infection, and other factors. In some cases, proper wound cleaning and dressing may be sufficient without the need for antiseptics.
FAQs
1. Can antiseptics be used on all types of wounds?
Antiseptics are not suitable for all types of wounds. For example, certain antiseptics, such as alcohol-based solutions, may cause irritation or delay healing in large open wounds. It’s important to choose the right antiseptic based on the wound type and consult a healthcare professional for severe wounds.
2. Are there natural alternatives to chemical antiseptics?
Yes, natural alternatives like honey, tea tree oil, and aloe vera have antimicrobial properties and can act as mild antiseptics. However, their effectiveness varies, and they may not be suitable for all situations or as effective as medical-grade antiseptics.
3. Can antiseptics contribute to antibiotic resistance?
While antiseptics themselves do not cause antibiotic resistance, improper use, such as overuse or misuse, can contribute to the development of resistant microorganisms. It’s important to use antiseptics appropriately to avoid contributing to this problem.
4. Are there any antiseptics safe for use on infants or young children?
Some antiseptics may not be safe for use on infants or young children due to their sensitive skin. For instance, chlorhexidine has been associated with skin burns in neonatal care. It is crucial to consult a healthcare professional before using any antiseptic on young children.
5. Can antiseptics be used in combination with antibiotics?
Yes, antiseptics can be used in conjunction with antibiotics, particularly in wound care, to reduce bacterial load and prevent infection. However, the combination should be guided by a healthcare professional to ensure effectiveness and avoid potential side effects.
6. What are the environmental impacts of using antiseptics?
The widespread use of antiseptics, particularly in healthcare and household settings, can have environmental impacts. Some antiseptic agents, like triclosan, have been found in water systems and may affect aquatic life. It’s important to dispose of antiseptic products properly to minimize environmental harm.
7. Can antiseptics be used for pets or animals?
Certain antiseptics are safe for use on pets or animals, but not all human antiseptics are suitable. For example, chlorhexidine is commonly used for pets, but it’s important to avoid using alcohol-based solutions as they can be toxic. Always consult a veterinarian before applying any antiseptic to pets.
8. Do antiseptics lose their effectiveness over time?
Yes, antiseptics can lose their effectiveness over time, especially if they are not stored properly. Factors like exposure to light, heat, and air can degrade antiseptic solutions, reducing their efficacy. Always check expiration dates and storage instructions.
9. Is there a difference in effectiveness between over-the-counter antiseptics and prescription antiseptics?
Over-the-counter antiseptics are generally formulated for minor cuts, scrapes, and burns, while prescription antiseptics may be stronger or designed for specific medical conditions. Prescription antiseptics are typically required for more severe or high-risk situations.
10. Can antiseptics be used on all body areas?
Not all antiseptics are suitable for use on all body areas. For example, some antiseptics may not be safe for use on mucous membranes, eyes, or certain sensitive skin areas. Always read product labels and consult a healthcare provider when in doubt.