Microflora refers to the diverse community of microorganisms that inhabit a specific environment, such as the human body or a particular ecosystem. In the context of human health, microflora primarily consists of bacteria, fungi, and other microorganisms that colonize various parts of the body, including the skin, mouth, and gastrointestinal tract. These microorganisms play crucial roles in maintaining overall health, supporting immune function, and aiding in digestion. The composition of microflora can vary significantly between individuals and can be influenced by factors such as diet, lifestyle, and environmental exposures. Imbalances in the microflora, known as dysbiosis, have been associated with various health conditions, including obesity and inflammatory disorders. Understanding the complex interactions between microflora and their host has become an important area of research in fields such as medicine, ecology, and biotechnology.
Distinction between microflora and microbiome
The terms “microflora” and “microbiome” are often used interchangeably, but they have distinct meanings. Microflora, now more commonly referred to as microbiota, specifically denotes the community of microorganisms, including bacteria, viruses, archaea, and fungi, that inhabit a particular environment, such as the human gut. On the other hand, the microbiome encompasses not only these microbial communities but also their collective genetic material, metabolic products, and the surrounding environmental conditions. This broader definition of the microbiome includes the functional potential and interactions of these microorganisms within their habitat, providing a more comprehensive understanding of their role in health and disease.
Types of Microflora
Microflora, also known as microbiota, are communities of microorganisms that inhabit various parts of the human body. These microorganisms play essential roles in maintaining health and preventing disease. Below are the different types of microflora:
1. Gut Microflora
The gut microflora, a complex and dynamic bacterial community, plays a crucial role in human health. It aids in digestion by salvaging energy and absorbable nutrients, and it has significant trophic effects on intestinal epithelia. The gut microflora also interacts with the immune system, influencing both innate and adaptive immunity, and helps in maintaining mucosal homeostasis. Dysbiosis, or imbalance in gut microflora, is linked to various diseases such as inflammatory bowel disease, colon cancer, and multisystem organ failure. Probiotics and prebiotics can be used to manipulate gut flora for therapeutic benefits.
2. Oral Microflora
Oral microflora consists of diverse bacterial species that play a vital role in maintaining oral health. These bacteria help in preventing colonization by pathogenic microbes, thus protecting against oral diseases such as dental caries and periodontal disease. The balance of oral microflora is crucial for preventing infections and maintaining overall oral health. Disruption in this balance can lead to oral diseases and contribute to systemic conditions.
3. Skin Microflora
The skin microflora, composed of various microorganisms, serves as a protective barrier against pathogenic bacteria and environmental threats. It plays a significant role in skin protection by maintaining the skin’s pH and producing antimicrobial substances. The skin microflora also influences the immune response and is involved in the development of skin conditions such as acne, eczema, and psoriasis. Maintaining a healthy skin microflora is essential for skin health and preventing infections.
4. Vaginal Microflora
Vaginal microflora, predominantly composed of Lactobacillus species, is crucial for female health. It maintains an acidic environment that inhibits the growth of pathogenic bacteria and yeast, thus preventing infections such as bacterial vaginosis and yeast infections. The balance of vaginal microflora is essential for reproductive health and preventing sexually transmitted infections. Disruption in this balance can lead to various gynecological issues.
5. Oral and Upper Respiratory Tract Microflora
The microflora of the oral and upper respiratory tract includes a variety of bacterial species that play a role in maintaining respiratory health. These microorganisms help in preventing colonization by pathogenic bacteria, thus reducing the risk of respiratory infections. The balance of microflora in these regions is crucial for preventing diseases such as pneumonia, sinusitis, and other respiratory conditions. Maintaining a healthy microflora in the oral and upper respiratory tract is essential for overall respiratory health.
Major Microflora Sites in the Human Body
Microflora are essential communities of microorganisms that inhabit various parts of the human body. These microorganisms play vital roles in maintaining health and preventing disease. Below are the major sites in the human body where microflora is found:
1. Skin
The skin is a major site for microbial colonization, hosting a diverse array of microorganisms, including bacteria, fungi, and viruses. The composition of the skin microbiota is influenced by various factors such as the local environment, host genetics, and immune responses. The skin’s microbiome plays a crucial role in protecting against pathogenic infections and maintaining skin health. However, under certain conditions, these commensal microorganisms can become pathogenic, leading to skin disorders. The skin microbiota is also involved in the development of the immune system and can influence systemic immune responses.
2. Oral Cavity/Upper Respiratory Tract
The oral cavity is one of the most diverse microbial habitats in the human body, second only to the gastrointestinal tract. It harbors over 700 bacterial species, along with fungi and viruses. The oral microbiome is crucial for maintaining oral health, but dysbiosis can lead to oral diseases such as periodontitis, caries, and oral cancer. Moreover, the oral microbiome has been linked to systemic diseases, including cardiovascular and respiratory diseases. The close connection between the oral cavity and the upper respiratory tract allows for the easy translocation of oral microbes, which can exacerbate respiratory conditions.
3. Gastrointestinal Tract
The gastrointestinal (GI) tract is the most densely populated microbial site in the human body, with the majority of microorganisms residing in the distal gut. The gut microbiota plays a vital role in digestion, nutrient absorption, and immune system development. Dysbiosis of the gut microbiota has been associated with various diseases, including inflammatory bowel disease, irritable bowel syndrome, and colorectal cancer. Additionally, the gut microbiota can influence the immune responses of distal organs, such as the lungs, thereby affecting respiratory health.
4. Vagina
The vaginal microbiota is predominantly composed of Lactobacillus species, which play a crucial role in maintaining vaginal health by producing lactic acid and maintaining a low pH environment. This microbiota composition can vary significantly throughout a woman’s life due to hormonal changes. Dysbiosis in the vaginal microbiota, such as bacterial vaginosis, can increase susceptibility to infections, including HIV. The vaginal microbiota also interacts with the immune system, providing protection against pathogens and contributing to reproductive health.
5. Urogenital Tract
The urogenital tract microbiota differs between men and women, with the female reproductive tract being more extensively studied. The lower urogenital tract is colonized by a variety of microorganisms, while the upper genital tract is generally considered sterile. The microbiota of the urogenital tract plays a role in preventing infections and maintaining mucosal immunity. Dysbiosis in this region can lead to conditions such as urinary tract infections and increased susceptibility to sexually transmitted infections.
6. Eyes
The eye microbiota is less diverse compared to other body sites but still plays a significant role in ocular health. The microorganisms present on the ocular surface help protect against pathogenic infections and maintain a balanced immune response. Disruption of the ocular microbiota can lead to conditions such as conjunctivitis and keratitis. The eye’s microbiome is influenced by factors such as age, environment, and contact lens use.
7. Respiratory Tract
The respiratory tract is colonized by a diverse array of microorganisms, including bacteria, fungi, and viruses. The upper respiratory tract, including the nasal passages and throat, has a more diverse microbiota compared to the lower respiratory tract. The respiratory microbiota plays a crucial role in protecting against respiratory infections and maintaining mucosal immunity. Dysbiosis in the respiratory microbiota has been linked to conditions such as asthma, chronic obstructive pulmonary disease (COPD), and respiratory infections.
Benefits of Microflora
Microflora is essential communities of microorganisms that inhabit various parts of the human body. These microorganisms play vital roles in maintaining health and preventing disease. Below are the key benefits of microflora and their specific functions:
1. Aiding Digestion
The gut microflora plays a crucial role in aiding digestion by breaking down complex carbohydrates and other indigestible compounds, thereby enhancing nutrient absorption and energy salvage. This metabolic activity is particularly significant in non-ruminants, where microbial activity in the lower gut helps in the degradation and synthesis of proteins, vitamins, and other essential nutrients. Additionally, the gut microflora participates in the absorption, distribution, metabolism, and excretion of nutrients, contributing to the host’s overall energy homeostasis. The presence of a balanced gut microflora ensures efficient digestion and nutrient utilization, which is vital for maintaining the host’s health.
2. Supporting Immune System
The gut microflora is integral to the development and function of the host’s immune system. It helps in the maturation of the immune system, particularly in early life, and maintains immune homeostasis throughout life. The interaction between gut microbiota and the immune system involves both innate and adaptive immune responses, which help in regulating inflammation and preventing infections. Probiotics, a component of gut microflora, have been shown to modulate immune responses, reduce gut dysbiosis, and minimize unnecessary activation of the immune system, thereby supporting overall immune health. This symbiotic relationship is essential for protecting the host from various pathogens and maintaining immune balance.
3. Synthesizing Essential Nutrients
Gut microflora is responsible for synthesizing several essential nutrients, including vitamins and amino acids. For instance, gut microorganisms synthesize vitamin K and B complex vitamins, which are crucial for various metabolic processes. They also play a role in the hydrogenation of polyunsaturated fatty acids and the transformation of bile acids and sterols, which are important for maintaining metabolic health. The synthesis of these nutrients by gut microflora not only supports the host’s nutritional needs but also contributes to the overall metabolic activity within the gastrointestinal tract. This microbial synthesis is particularly beneficial for individuals with low dietary intake of these essential nutrients.
4. Protecting Against Harmful Pathogens
The gut microflora provides a protective barrier against harmful pathogens by maintaining a balanced microbial ecosystem. This balance prevents the colonization and invasion of pathogenic bacteria, thereby reducing the risk of infections. The presence of beneficial bacteria, such as probiotics, enhances this protective effect by competing with pathogenic microbes for resources and space, producing antimicrobial substances, and modulating the host’s immune responses. Additionally, a healthy gut microflora can prevent dysbiosis, which is associated with increased susceptibility to infections and other health issues. By maintaining a stable and diverse microbial community, the gut microflora plays a critical role in protecting the host from various pathogenic threats.
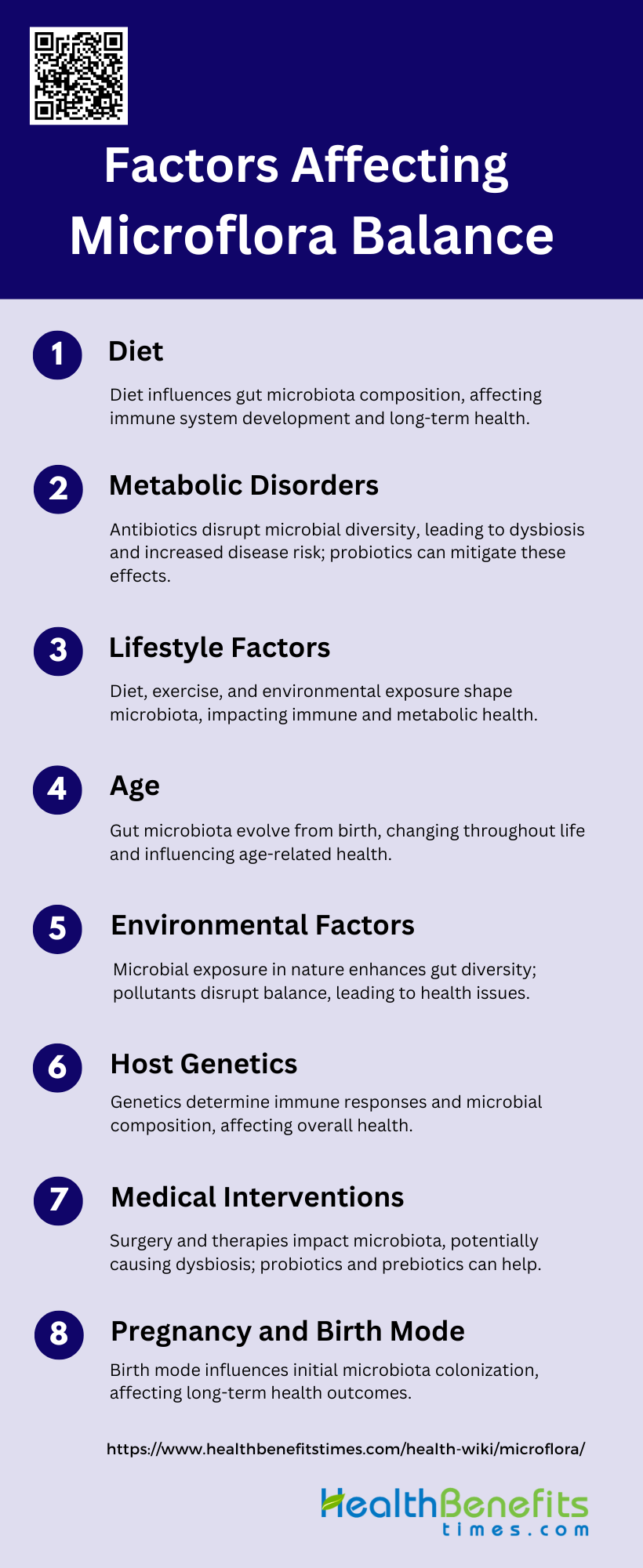
Factors Affecting Microflora Balance
Microflora is essential communities of microorganisms that inhabit various parts of the human body. Their balance can be influenced by various factors, impacting overall health. Below is the key factors affecting microflora balance:
1. Diet
Diet plays a crucial role in shaping the gut microbiota. Maternal diet, particularly during pregnancy, can influence the initial colonization of the infant gut microbiota, which is critical for the development of the immune system and metabolic homeostasis. Postnatal diet, including breastfeeding and the introduction of solid foods, further modulates the microbial diversity and composition in the gut. Nutritional stresses during early life can alter the initial colonizing bacteria and the development of signaling pathways controlled by microbial mediators, potentially setting the stage for long-term metabolic and immune health. Therefore, dietary interventions are considered a promising strategy to modulate gut microbiota and improve health outcomes.
2. Antibiotics
Antibiotics significantly impact the composition and diversity of the gut microbiota. Prenatal and neonatal exposure to antibiotics can disrupt the initial colonization of the infant gut, leading to a state of dysbiosis, which is associated with an increased risk of diseases such as obesity, diabetes, and allergies later in life. Antibiotic treatment can reduce microbial diversity and alter the balance of beneficial and harmful bacteria, potentially leading to long-term health consequences. Strategies to mitigate the adverse effects of antibiotics on the gut microbiota include the use of probiotics, prebiotics, and fecal microbiota transplantation.
3. Lifestyle Factors
Lifestyle factors, including diet, physical activity, and exposure to the natural environment, significantly influence the composition of the gut microbiota. These factors can modulate interrelated physiological systems, such as the immune system, metabolic pathways, and brain function. For instance, a diet rich in fiber and low in processed foods promotes a healthy gut microbiota, while a sedentary lifestyle and poor dietary habits can lead to dysbiosis and associated health issues. Additionally, exposure to diverse environmental microbes can enhance microbial diversity and contribute to better health outcomes.
4. Age
Age is a critical factor affecting the gut microbiota. The initial colonization of the gut microbiota occurs at birth and continues to develop dynamically until it reaches a stable, adult-like composition by the age of three. Throughout life, the gut microbiota undergoes changes influenced by diet, lifestyle, and environmental factors. In older adults, a decline in microbial diversity is often observed, which can be associated with age-related health issues such as inflammation and metabolic disorders. Understanding the age-related changes in gut microbiota can help develop targeted interventions to maintain a healthy microbiota throughout life.
5. Environmental Factors
Environmental factors, including exposure to microbes in the natural environment, play a significant role in shaping the gut microbiota. Contact with diverse microbial communities in soil, water, and plants can enhance the diversity and resilience of the gut microbiota. Environmental pollutants and chemicals, on the other hand, can disrupt the microbial balance and contribute to dysbiosis. The interplay between environmental microbial ecosystems and the human microbiota highlights the importance of considering environmental health in strategies to promote human health.
6. Host Genetics
Host genetics influence the composition and function of the gut microbiota. Genetic factors can determine the host’s immune response, production of antimicrobial peptides, and other mechanisms that shape the microbial community in the gut. Studies have shown that specific genetic variations can affect the abundance of certain microbial taxa and their metabolic activities. Understanding the genetic basis of host-microbiota interactions can provide insights into personalized approaches to modulate the gut microbiota for improved health outcomes.
7. Medical Interventions
Medical interventions, such as surgery, chemotherapy, and immunotherapy, can significantly impact the gut microbiota. These interventions can disrupt the microbial balance, leading to dysbiosis and associated health complications. For example, chemotherapy can reduce microbial diversity and alter the gut microbiota composition, affecting the patient’s immune response and overall health. Strategies to mitigate the adverse effects of medical interventions on the gut microbiota include the use of probiotics, prebiotics, and fecal microbiota transplantation.
8. Pregnancy and Birth Mode
Pregnancy and birth mode are critical factors influencing the initial colonization of the infant gut microbiota. The maternal microbiota forms the first microbial inoculum for the infant, and factors such as maternal diet, antibiotic use, and mode of delivery (vaginal birth vs. cesarean section) can shape the newborn’s microbiota. Vaginally delivered infants are exposed to maternal vaginal and gut microbiota, while cesarean-delivered infants are more likely to be colonized by skin and environmental microbes. These early microbial exposures can have long-term implications for the infant’s immune system development and health outcomes.
Health Issues of Microflora Imbalances
Microflora is essential communities of microorganisms that inhabit various parts of the human body. Imbalances in these communities can lead to a range of health issues. Below are the key health issues associated with microflora imbalances:
1. Gastrointestinal Disorders
Gastrointestinal disorders are closely linked to imbalances in the gut microflora, a condition known as dysbiosis. Dysbiosis can lead to various gastrointestinal diseases such as Crohn’s disease, irritable bowel syndrome (IBS), and small intestine bacterial overgrowth (SIBO). These conditions are often characterized by an imbalance between beneficial and harmful bacteria, leading to inflammation and impaired gut function. For instance, Crohn’s disease has been associated with a reduction in beneficial microbial populations and an increase in pathogenic bacteria, which can exacerbate intestinal inflammation and damage. Treatment strategies often focus on restoring microbial balance through probiotics, prebiotics, and dietary interventions.
2. Metabolic Disorders
The gut microflora plays a significant role in the development of metabolic disorders such as obesity, type 1 diabetes, and nonalcoholic fatty liver disease. Dysbiosis in the gut can disrupt metabolic homeostasis by affecting lipid and carbohydrate metabolism, energy balance, and insulin sensitivity. For example, an abundance of proinflammatory microbes and a lack of butyrate-producing strains can lead to chronic low-grade inflammation, which is a common feature in metabolic disorders. Recent studies have shown that manipulating the gut microflora through probiotics and dietary changes can help in managing these conditions by restoring a healthy microbial balance.
3. Immune System Disorders
The gut microflora is crucial for the normal development and function of the mucosal immune system. Dysbiosis can lead to immune system disorders by disrupting the delicate balance between commensal and pathogenic bacteria, resulting in inappropriate immune responses. In genetically susceptible individuals, this imbalance can contribute to the pathogenesis of inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis. The gut microflora’s role in modulating immune responses highlights the potential of probiotics and prebiotics as therapeutic strategies to enhance beneficial microbial components and mitigate harmful ones.
4. Neurological and Mental Health Issues
The gut-brain axis is a bidirectional communication system between the gut microflora and the brain, influencing neurological and mental health. Dysbiosis has been implicated in various neurological disorders, including depression, autism, Alzheimer’s disease, and Parkinson’s disease. The gut microflora can affect brain function through the production of neuroactive compounds, modulation of the immune system, and alteration of the gut barrier integrity. For instance, an imbalance in gut bacteria can lead to increased production of proinflammatory cytokines, which can affect brain function and contribute to neurodegenerative diseases3. Probiotic treatments aimed at restoring healthy gut microflora diversity have shown promise in alleviating some of these conditions.
5. Skin Conditions
The gut microflora also plays a role in skin health, with dysbiosis being linked to various skin conditions such as acne, eczema, and psoriasis. The gut-skin axis involves complex interactions between the gut microflora, immune system, and skin barrier function. Dysbiosis can lead to increased intestinal permeability, allowing microbial metabolites and toxins to enter the bloodstream and trigger inflammatory responses in the skin. Probiotics and dietary interventions that promote a healthy gut microflora have been shown to improve skin conditions by reducing inflammation and enhancing skin barrier function.
Maintaining Healthy Microflora
Maintaining a healthy microflora is essential for overall well-being. The balance of beneficial bacteria in our gut influences digestion, immunity, and even mental health. Here are some key practices to help maintain a healthy microflora:
1. Eat a diverse, balanced diet
A diverse and balanced diet is crucial for maintaining a healthy gut microbiota. Consuming a variety of foods, especially those rich in vegetable fiber, omega-3 polyunsaturated fatty acids, vitamins D and E, and other micronutrients, can enhance the biodiversity of the gut microbiota. This diversity is essential for the production of short-chain fatty acids, which play a significant role in gut health. A diet high in processed foods, refined sugars, and unhealthy fats, typical of Western diets, can lead to gut dysbiosis and associated health issues such as obesity and intestinal inflammation.
2. Consume probiotic foods
Probiotic foods, such as yogurt, kefir, and fermented vegetables, can positively influence gut microbiota by introducing beneficial bacteria. These foods help maintain a balanced microbial environment in the gut, which is essential for overall health. The intake of probiotics can vary in effectiveness due to inter- and intra-individual factors, but they generally support the growth of beneficial bacteria and inhibit harmful pathogens. Regular consumption of probiotic foods can help prevent gut dysbiosis and improve digestive health.
3. Stay hydrated
Staying hydrated is essential for maintaining a healthy gut microbiota. Adequate water intake supports the mucosal lining of the intestines and the balance of good bacteria in the gut. Hydration helps in the digestion and absorption of nutrients, which in turn supports the growth of beneficial gut bacteria. Dehydration can lead to constipation and an imbalance in gut microbiota, potentially causing gut dysbiosis. Therefore, drinking sufficient water daily is a simple yet effective way to support gut health.
4. Manage stress
Chronic psychological stress can negatively impact gut microbiota, leading to gut dysbiosis and related health issues. Stress can alter the gut-brain axis, affecting the composition and function of gut bacteria. Managing stress through techniques such as mindfulness, meditation, and regular physical activity can help maintain a healthy gut microbiota. Reducing stress levels can improve gut health by promoting a balanced microbial environment and preventing the overgrowth of harmful bacteria and fungi.
5. Exercise regularly
Regular physical activity is beneficial for gut health as it promotes a diverse and balanced gut microbiota. Exercise has been shown to increase the abundance of beneficial bacteria and reduce the prevalence of harmful bacteria. It also helps in the production of short-chain fatty acids, which are crucial for gut health. A sedentary lifestyle, on the other hand, is associated with gut dysbiosis and related health issues. Therefore, incorporating regular exercise into your routine can significantly improve gut microbiota composition and overall health.
6. Get enough sleep
Adequate sleep is essential for maintaining a healthy gut microbiota. Poor sleep quality and sleep deprivation can disrupt the balance of gut bacteria, leading to gut dysbiosis. Sleep is crucial for the regulation of the gut-brain axis, which influences gut health. Ensuring sufficient and quality sleep can help maintain a balanced microbial environment in the gut, supporting overall health and well-being. Therefore, prioritizing good sleep hygiene is important for gut health.
7. Limit antibiotic use
While antibiotics are necessary for treating bacterial infections, their overuse can disrupt the balance of gut microbiota. Antibiotics can kill both harmful and beneficial bacteria, leading to gut dysbiosis. Limiting the use of antibiotics to when they are absolutely necessary can help preserve the beneficial bacteria in the gut. When antibiotics are required, taking probiotic supplements or consuming probiotic foods can help restore the balance of gut microbiota.
8. Consider probiotic supplements
Probiotic supplements can be beneficial for maintaining a healthy gut microbiota, especially when dietary intake of probiotic foods is insufficient. These supplements contain live beneficial bacteria that can help restore and maintain the balance of gut microbiota. They are particularly useful after antibiotic treatment or during periods of stress, poor diet, or illness. However, the response to probiotic supplements can vary among individuals, so it is important to choose high-quality products and consult with a healthcare provider.
9. Avoid excessive alcohol consumption
Excessive alcohol consumption can negatively impact gut microbiota, leading to gut dysbiosis and associated health issues. Alcohol can disrupt the balance of beneficial and harmful bacteria in the gut, promoting the growth of pathogenic bacteria and fungi. Limiting alcohol intake can help maintain a healthy gut microbiota and prevent related health problems. Moderation is key, as occasional and moderate alcohol consumption is less likely to cause significant harm to gut health.
10. Don’t smoke
Smoking has been shown to negatively affect gut microbiota, leading to gut dysbiosis and increased risk of gastrointestinal diseases. The harmful chemicals in tobacco smoke can alter the composition of gut bacteria, reducing the abundance of beneficial bacteria and promoting the growth of harmful ones. Quitting smoking can significantly improve gut health by restoring a balanced microbial environment. Therefore, avoiding smoking is crucial for maintaining a healthy gut microbiota and overall health.
FAQs
1. How do microflora and microbiome differ in their impact on health?
Microflora refers to the specific community of microorganisms living in a particular environment (like the gut or skin), while the microbiome includes these microorganisms and their collective genetic material, functions, and interactions with the host. The microbiome, therefore, has a broader impact on health as it encompasses not just the microorganisms themselves but also their roles in metabolism, immune modulation, and overall homeostasis.
2. What are some common signs of an imbalanced microflora?
Signs of an imbalanced microflora (dysbiosis) can include digestive issues like bloating, gas, and diarrhea; skin problems such as acne or eczema; frequent infections; fatigue; and even mood disturbances like anxiety or depression.
3. How does the use of probiotics differ from prebiotics in maintaining microflora balance?
Probiotics are live beneficial bacteria that can help replenish and maintain healthy microflora, while prebiotics are non-digestible fibers that serve as food for these beneficial bacteria, promoting their growth and activity in the gut. Both are used to support a balanced microbiota, but they work in complementary ways.
4. Can genetics affect the composition of my microflora?
Yes, genetics can influence the composition and diversity of an individual’s microflora. Genetic factors may determine how the body interacts with different microorganisms, including the production of specific immune molecules that shape the microbial community in various body sites.
5. How do hormonal changes during pregnancy affect vaginal microflora?
Hormonal changes during pregnancy, particularly the increase in estrogen, can influence the composition of vaginal microflora by promoting the growth of Lactobacillus species, which help maintain an acidic environment and protect against infections. However, these changes can also make the vaginal microflora more susceptible to imbalances if disrupted.
6. Is there a connection between oral microflora and heart health?
Yes, there is evidence linking oral microflora to heart health. Poor oral hygiene and an imbalance in oral microflora can lead to gum disease, which has been associated with an increased risk of cardiovascular diseases. This is believed to be due to bacteria from the mouth entering the bloodstream and contributing to inflammation and plaque buildup in the arteries.
7. What are some natural ways to restore microflora balance after antibiotic use?
Natural ways to restore microflora balance after antibiotic use include consuming probiotic-rich foods (like yogurt, kefir, and sauerkraut), prebiotic-rich foods (such as garlic, onions, and bananas), staying hydrated, managing stress, and avoiding processed foods and sugars that can promote harmful bacteria growth.
8. Can changes in microflora affect mental health, and if so, how?
Yes, changes in microflora can affect mental health through the gut-brain axis, a communication network linking the gut and the brain. Dysbiosis can lead to increased inflammation, altered neurotransmitter production, and changes in mood and behavior, contributing to conditions like anxiety and depression.
9. How does age affect the diversity of microflora in different parts of the body?
Age significantly affects microflora diversity. In infants, microflora diversity is relatively low and changes rapidly with diet and environmental exposures. In adults, diversity reaches a stable state but can decrease with age, especially in elderly individuals, potentially impacting health due to reduced microbial diversity and resilience.
10. What role does microflora play in allergy development or prevention?
Microflora can influence the development or prevention of allergies by modulating the immune system. A balanced microflora can help regulate immune responses and prevent overreactive responses to allergens. Conversely, an imbalanced microflora (dysbiosis) may increase susceptibility to allergies by disrupting normal immune tolerance.