Helminths are parasitic worms that can infect humans and animals, causing various health issues. These multicellular organisms belong to several phyla, including Nematoda (roundworms), Platyhelminthes (flatworms), and Acanthocephala (thorny-headed worms). Helminths can inhabit different parts of the host’s body, but they commonly reside in the gastrointestinal tract. These parasites have complex life cycles, often involving multiple hosts, and can be transmitted through contaminated soil, water, food, or direct contact with infected individuals or animals. Helminth infections can lead to a range of symptoms, from mild discomfort to severe malnutrition and organ damage, depending on the species and intensity of infection. Some common examples of helminths include Ascaris lumbricoides (roundworm), Trichuris trichiura (whipworm), and various species of tapeworms.
Types of Helminths
Helminths are parasitic worms that can infect humans and animals, causing various health issues. There are three main types of helminths:
1. Nematodes (Roundworms)
Nematodes, also known as roundworms, are a diverse group of parasitic worms with over 300 types known to infect humans. These worms have cylindrical bodies and can cause a range of ailments and diseases. Some common examples include Ascaris lumbricoides (intestinal roundworm) and Trichinella spiralis (causes trichinosis). Nematode infections can lead to malnutrition, intestinal obstruction, and impaired growth in children. Fortunately, effective anthelmintic medications are available to treat these infections, although their impact on global health remains significant.
2. Cestodes (Tapeworms)
Cestodes, or tapeworms, are flat, ribbon-like parasites that inhabit the intestines of their hosts. These helminths have a complex life cycle, often involving multiple hosts. Common examples include Taenia solium (pork tapeworm) and Echinococcus granulosus (causes hydatid disease). Tapeworm infections can cause abdominal pain, weight loss, and nutrient deficiencies. In severe cases, larval stages of some tapeworms can migrate to other organs, leading to potentially life-threatening conditions. Cestode infections are particularly prevalent in regions with poor sanitation and inadequate meat inspection practices.
3. Trematodes (Flukes)
Trematodes, also called flukes, are flat, leaf-shaped parasites that can infect various organs in humans. These helminths have complex life cycles involving intermediate hosts such as snails and fish. Common examples include Schistosoma species (cause schistosomiasis) and Clonorchis sinensis (Chinese liver fluke). Trematode infections can lead to chronic inflammation, organ damage, and in some cases, increased risk of cancer. Foodborne trematodes alone affect an estimated 80 million people worldwide, with the highest prevalence in Asia. Control efforts focus on improving sanitation, food safety, and providing targeted treatment to affected populations.
Lifecycle of Helminths
General Lifecycle Stages
The lifecycle of soil-transmitted helminths (STHs) typically involves several stages. It begins with eggs or larvae being released into the environment through infected human feces. These eggs or larvae then develop in soil under suitable conditions. When humans come into contact with contaminated soil, the infective stage of the parasite can penetrate the skin or be ingested. Once inside the human host, the parasites migrate to their preferred location in the body, mature into adult worms, and reproduce. Adult female worms then lay eggs, which are excreted in feces, completing the cycle. This basic pattern is common to most STHs, although the specific details can vary between species.
Differences Between Lifecycle Stages of Each Type
Different STH species have unique lifecycle characteristics. Hookworms (Necator americanus and Ancylostoma duodenale) typically penetrate the skin and migrate through the bloodstream to the lungs before being coughed up and swallowed. Whipworms (Trichuris trichiura) and roundworms (Ascaris lumbricoides) are usually ingested as eggs and develop directly in the intestines. Strongyloides stercoralis, the threadworm, can complete its entire lifecycle within the human host through a process called autoinfection. Ascaris eggs can survive on produce and hands, potentially contributing to transmission. Some species, like Ostertagia gruehneri in caribou, can undergo arrested development in the host as a survival strategy.
Transmission Methods
STHs employ various transmission methods. The most common route is through contaminated soil, hence the name “soil-transmitted”. Eggs or larvae in soil can be ingested through unwashed hands, contaminated food (especially raw fruits and vegetables), or drinking water. Some species, like hookworms, can actively penetrate the skin when people walk barefoot on contaminated soil. Poor sanitation and hygiene practices contribute significantly to transmission. In some cases, such as with Strongyloides, autoinfection can occur, where larvae develop and reinfect the host without leaving the body. Climate and environmental factors can influence transmission patterns, affecting the survival and development of free-living stages.
Helminths in Humans
Common Helminth Infections
Helminth infections are prevalent worldwide, with soil-transmitted helminths (STH) being the most common. The most frequent STH infections in humans are caused by Ascaris lumbricoides (roundworm), Trichuris trichiura (whipworm), and hookworms. Other significant helminth infections include schistosomiasis, caused by blood flukes of the genus Schistosoma, and strongyloidiasis, caused by Strongyloides stercoralis. These parasitic worms can infect various parts of the human body, with intestinal infections being the most common. The prevalence of helminth infections varies by region, with higher rates typically found in tropical and subtropical areas, particularly in communities with poor sanitation and hygiene practices.
Symptoms and Health Implications
Helminth infections can range from asymptomatic to severe, depending on the parasite load and the host’s immune response. Common symptoms include abdominal pain, diarrhea, malnutrition, and anemia. In children, chronic infections can lead to impaired growth and cognitive development. Severe cases may cause intestinal obstruction, rectal prolapse, or organ damage. Some helminths, like Strongyloides stercoralis, can cause hyperinfection syndrome in immunocompromised individuals, leading to potentially fatal outcomes. Helminth infections can also modulate the host’s immune system, potentially affecting responses to other infections and allergic diseases. The overall impact on public health is significant, with helminthiasis being one of the most common infectious diseases globally.
How Infections Occur
Helminth infections typically occur through contact with contaminated soil, water, or food. Soil-transmitted helminths are often acquired by ingesting eggs from contaminated soil or consuming unwashed vegetables grown in contaminated soil. Some helminths, like hookworms, can penetrate the skin when walking barefoot on contaminated soil. Schistosomiasis is contracted through contact with freshwater contaminated with larval forms of the parasite. Poor sanitation, lack of access to clean water, and inadequate hygiene practices contribute significantly to the transmission of these parasites. In some cases, such as strongyloidiasis, the parasite can persist through autoinfection, where larvae develop and reinfect the host without leaving the body. Maternal infections during pregnancy can also increase the risk of early childhood infections.
Common symptoms of helminth infections
Helminth infections can cause a wide range of symptoms, often depending on the specific parasite and the location of infection within the body. While some infections may be asymptomatic, many individuals experience various discomforts and health issues. The following list outlines some of the most common symptoms associated with helminth infections:
- Abdominal pain and diarrhea
- Loss of appetite
- Fatigue
- Anemia
- Muscle and joint pain
- Cough
- Shortness of breath
- Itching and Rashes
- Headaches
- Seizures
- Eosinophilia (increased eosinophil count in blood)
- Growth stunting in children
- Hives
Diagnosis of Helminth Infections
The accurate diagnosis of helminth infections is crucial for effective treatment and control programs. Various diagnostic methods are available, each with its own strengths and limitations. Here’s are the diagnostic techniques used for detecting helminth infections:
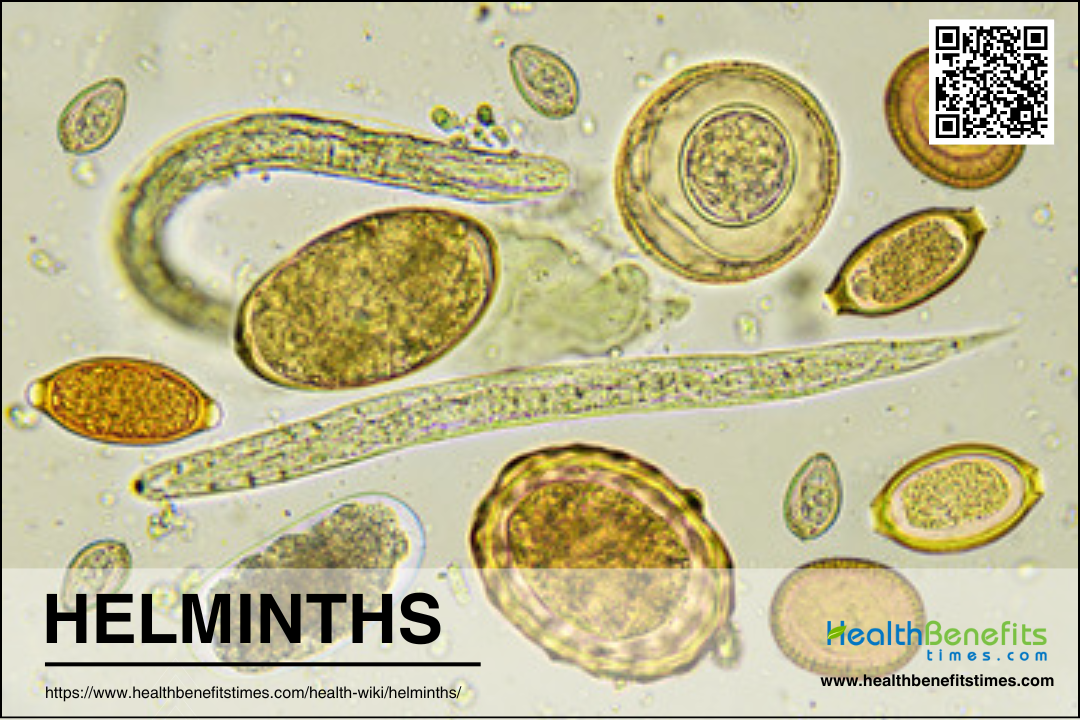
1. Microscopy-Based Methods
Microscopy remains the most widely used method for diagnosing helminth infections, particularly in resource-limited settings. The Kato-Katz (KK) thick smear technique is the most common microscopy-based method. It involves examining a small amount of stool under a microscope to identify and count helminth eggs. While KK is inexpensive and relatively simple to perform, it lacks sensitivity in detecting low-intensity infections. Other microscopy-based methods include:
- Direct wet mount microscopy
- McMaster technique
- Spontaneous tube sedimentation
2. Molecular Diagnostic Techniques
Molecular methods, particularly quantitative polymerase chain reaction (qPCR), are becoming increasingly popular for helminth diagnosis due to their higher sensitivity. Multiplex qPCR can detect multiple helminth species simultaneously and is especially useful in low-prevalence settings or when infection intensities are low. This method has shown significantly higher detection rates compared to microscopy-based techniques for various helminth species, including Ascaris lumbricoides and Trichuris trichiura.
Treatment methods for Helminths
Helminth infections, caused by parasitic worms, are a significant public health concern, particularly in tropical and subtropical regions. Effective treatment involves a combination of medical interventions and supportive measures. Below are the primary methods used to treat helminth:
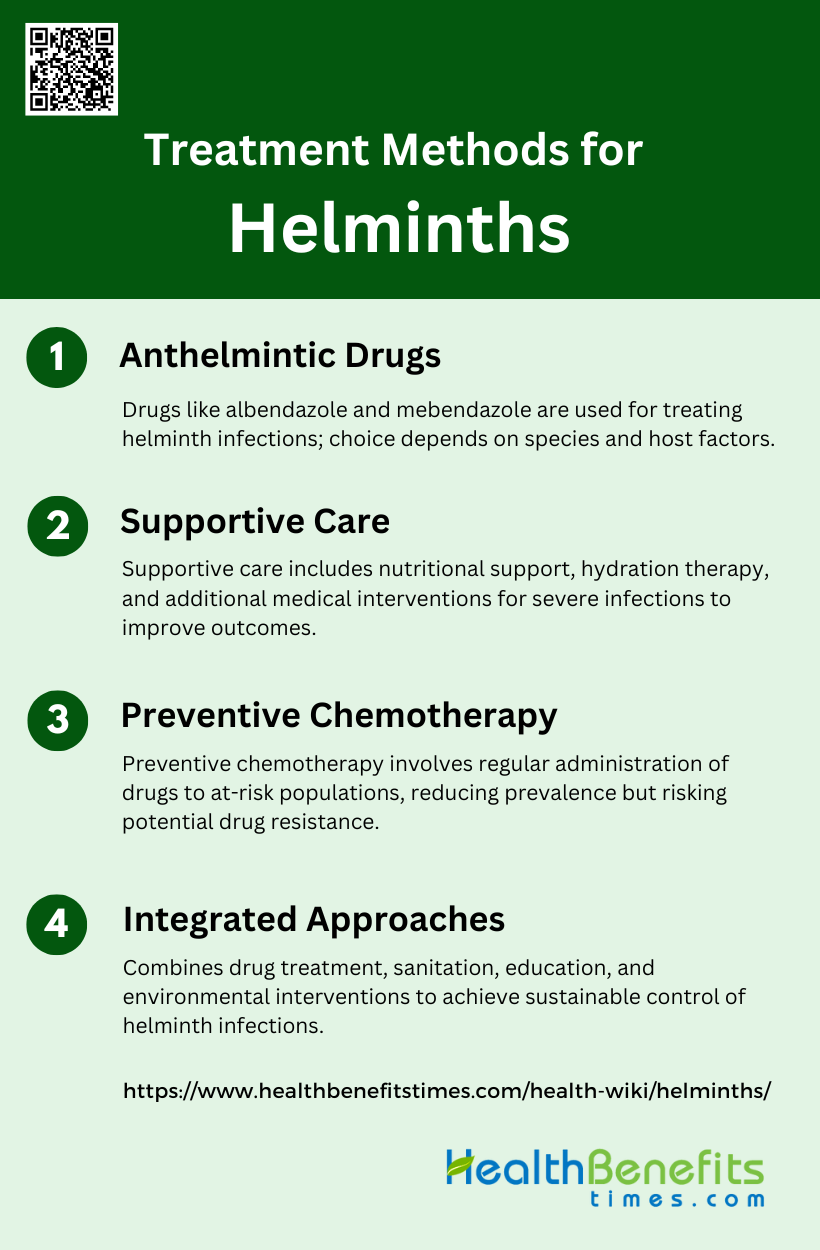
1. Anthelmintic Drugs
Anthelmintic drugs are the primary treatment method for helminth infections. Albendazole is a widely used anthelmintic, effective against various soil-transmitted helminths (STH) such as Ascaris lumbricoides, Trichuris trichiura, and hookworms. A triple dose of albendazole (400mg daily for 3 days) has shown high cure rates and egg reduction rates for most STH species. Fenbendazole, another anthelmintic, has demonstrated excellent efficacy against common nematodes in dogs when administered at 50 mg/kg of body weight daily for 3 days. Mebendazole is also used but may have lower cure rates compared to albendazole for some helminth species. The choice of anthelmintic and dosing regimen depends on the specific helminth species and host factors.
2. Supportive Care
Supportive care is an essential component of helminth treatment, addressing the symptoms and complications associated with these infections. This may include nutritional support to combat malnutrition caused by intestinal parasites, iron supplementation for anemia, and hydration therapy for diarrheal symptoms. In cases of severe infections, additional medical interventions may be necessary to manage complications such as intestinal obstruction or organ damage. Supportive care is particularly crucial for vulnerable populations like pre-school age children and pregnant women, who are at higher risk of morbidity from helminth infections. The goal of supportive care is to alleviate symptoms, prevent complications, and improve overall health outcomes for infected individuals.
3. Preventive Chemotherapy
Preventive chemotherapy (PC) is a key strategy in controlling helminth infections at the population level. This approach involves the periodic administration of anthelmintic drugs to at-risk populations, typically without individual diagnosis. The World Health Organization recommends PC for school-age children in endemic areas to reduce the prevalence of moderate-to-heavy infections. The frequency and duration of PC depend on the baseline prevalence of infection in the target population. However, there are concerns about the potential development of drug resistance with long-term PC programs. To monitor the effectiveness of PC, periodic surveys are conducted in sentinel villages to assess infection levels and determine when treatment can be safely stopped.
4. Integrated Approaches
Integrated approaches combine multiple strategies to effectively control and prevent helminth infections. These may include anthelmintic treatment, improved sanitation, health education, and environmental interventions. For example, studies in indigenous communities have shown that factors such as lack of latrines and indiscriminate defecation are associated with higher STH infection rates. Addressing these issues through improved water, sanitation, and hygiene (WASH) practices can complement drug-based interventions. Additionally, integrated approaches may involve targeting multiple parasites simultaneously, as co-infections are common in endemic areas. Metabolomic studies are emerging as a promising tool to understand the complex interactions between helminths, hosts, and the microbiome, potentially leading to new integrated control strategies.
Prevention and Control of Helminth
Preventing and controlling helminth infections is crucial for reducing their impact on public health. Effective strategies involve a combination of medical treatments, public health initiatives, and community education. Below are the key methods for preventing and controlling helminth:
1. Preventive Chemotherapy
Preventive chemotherapy is a cornerstone in the control of helminth infections. It involves the administration of anthelmintic drugs to at-risk populations, particularly school-aged children. Mass drug administration (MDA) campaigns using praziquantel and albendazole are widely implemented in endemic areas. While effective in reducing infection rates, MDA alone does not prevent reinfection. The frequency and coverage of preventive chemotherapy are crucial factors in its success. However, potential adverse events should be monitored, especially in preschool-aged children who may be more susceptible to side effects.
2. Improved Sanitation and Hygiene
Improving sanitation and hygiene practices is essential for long-term helminth control. This approach addresses the root causes of infection by reducing environmental contamination with helminth eggs. Proper sanitation facilities, such as latrines and clean water sources, help break the transmission cycle. Promoting handwashing with soap, especially before meals and after using the toilet, can significantly reduce the risk of infection. Improved sanitation not only helps control helminths but also contributes to overall public health and community well-being.
3. Health Education
Health education plays a vital role in helminth prevention and control. School-based health education packages, such as “The Magic Glasses,” have shown promise in increasing knowledge and promoting behavior change. These programs aim to teach children about helminth transmission, symptoms, and prevention methods. Effective health education should be culturally appropriate and age-specific. By empowering communities with knowledge, health education can lead to sustainable changes in practices that reduce helminth transmission and reinfection rates.
4. Integrated Approach
An integrated approach to helminth control combines multiple strategies for maximum impact. This includes preventive chemotherapy, improved sanitation, health education, and other complementary measures. By addressing various aspects of helminth transmission and infection simultaneously, an integrated approach can achieve more sustainable results than any single intervention alone. This strategy recognizes the complex nature of helminth infections and the need for comprehensive solutions that target both immediate treatment and long-term prevention.
5. Vector Control
Vector control is crucial for preventing helminth infections transmitted by intermediate hosts or vectors. For example, controlling snail populations is essential in the fight against schistosomiasis. Vector control methods may include chemical treatments, biological control agents, or environmental modifications that reduce vector habitats. Effective vector control requires a thorough understanding of local ecology and vector biology. When implemented alongside other prevention strategies, vector control can significantly reduce transmission rates and contribute to long-term helminth control.
6. Environmental Interventions
Environmental interventions focus on modifying the physical environment to reduce helminth transmission. This can include improving water management systems, implementing proper waste disposal methods, and promoting agricultural practices that minimize soil contamination. Environmental interventions often require collaboration between health, agriculture, and water management sectors. By creating an environment less conducive to helminth survival and transmission, these interventions can have a lasting impact on infection rates and community health.
7. Monitoring and Evaluation
Regular monitoring and evaluation are essential components of effective helminth control programs. This involves conducting parasitological surveys to assess infection rates, evaluating the impact of interventions, and identifying emerging hotspots. High-resolution data at the sub-district or village level can reveal localized areas of high transmission that may be missed by district-level assessments. Continuous monitoring allows for timely adjustments to control strategies and helps ensure that resources are allocated efficiently to areas of greatest need.
8. Community-led Initiatives
Community-led initiatives empower local populations to take an active role in helminth control. These programs involve community members in planning, implementing, and evaluating control measures. By fostering a sense of ownership and responsibility, community-led initiatives can lead to more sustainable outcomes. Local knowledge and cultural practices can be integrated into control strategies, increasing their acceptability and effectiveness. Engaging community leaders and volunteers can also help extend the reach of prevention efforts and promote long-term behavior change.
Interesting Facts about Helminths
Helminths have fascinating biological characteristics and significant impacts on human health and ecosystems. These organisms have adapted to survive in various hosts and environments. Below are some interesting facts about helminths:
1. Ancient parasites
Helminths have been parasitizing animals for millions of years, with evidence of their existence dating back to prehistoric times. Fossilized helminth eggs have been discovered in ancient coprolites (fossilized feces) from dinosaurs and early mammals. These parasites have co-evolved with their hosts over millennia, developing intricate relationships and adaptations. Their long evolutionary history has allowed helminths to become highly specialized and efficient parasites.
2. Widespread prevalence
Helminths are incredibly common parasites, infecting a wide range of hosts across the animal kingdom. They can be found in both terrestrial and aquatic environments, affecting vertebrates and invertebrates alike. In fact, helminths are so prevalent that they infect nearly every species of wild animal. Even in human populations, helminth infections remain a significant global health concern, particularly in developing countries where sanitation and healthcare access may be limited.
3. Complex life cycles
Many helminth species have intricate life cycles that involve multiple hosts and stages of development. For example, some tapeworms require two or more intermediate hosts before reaching their final host. These complex life cycles often include remarkable transformations, with larvae undergoing dramatic morphological changes as they move from one host to another. This complexity allows helminths to exploit various ecological niches and increase their chances of survival and reproduction.
4. Host manipulation
Some helminths have evolved the ability to manipulate their hosts’ behavior to facilitate their own transmission. This fascinating adaptation can lead to altered host behavior that increases the likelihood of the parasite being transmitted to its next host. For instance, certain parasites can cause infected prey animals to become more susceptible to predation, thereby ensuring the parasite’s life cycle continues. This manipulation demonstrates the profound impact helminths can have on their hosts and ecosystems.
5. Impressive reproductive capacity
Helminths are known for their extraordinary reproductive abilities. Many species can produce thousands of eggs daily, with some capable of laying millions over their lifetime. This high reproductive output is an adaptation to overcome the challenges of their complex life cycles and ensure successful transmission to new hosts. The sheer number of offspring produced by helminths contributes to their widespread prevalence and persistence in various environments.
6. Size extremes
Helminths exhibit a remarkable range in size, from microscopic to impressively large. Some species, like certain nematodes, can be less than a millimeter long, while others, such as tapeworms, can grow to extraordinary lengths. The fish tapeworm (Diphyllobothrium latum) holds the record for the longest known parasite, capable of reaching lengths of up to 30 meters (98 feet) inside its host. This size diversity allows helminths to occupy various niches within their hosts.
7. Longevity
Certain helminth species are known for their impressive longevity. Some can survive for decades within their hosts, continuously reproducing and causing chronic infections. For example, the guinea worm (Dracunculus medinensis) can live in the human body for up to 14 months before emerging. This long lifespan allows helminths to persist in host populations and potentially cause long-term health effects in infected individuals.
8. Diverse habitats
Helminths have adapted to inhabit a wide range of environments within their hosts. They can be found in various organs and tissues, including the intestines, liver, lungs, blood vessels, and even the brain. Some species, like Leucochloridium variae, parasitize the cloaca of birds. This diversity in habitat preferences demonstrates the remarkable adaptability of helminths and their ability to exploit different resources within their hosts.
9. Zoonotic potential
Many helminth species have zoonotic potential, meaning they can be transmitted from animals to humans. This characteristic makes them important from a public health perspective. Zoonotic helminths can cause various diseases in humans, ranging from mild to severe. Understanding the zoonotic potential of helminths is crucial for developing effective control strategies and preventing the spread of these parasites between animals and humans.
FAQs
1. Can helminth infections be prevented by dietary changes?
While the article mentions sanitation and hygiene as prevention methods, it does not address whether certain dietary practices can help prevent helminth infections, such as consuming cooked food only, avoiding raw or undercooked meat, or including specific anti-parasitic foods like garlic or pumpkin seeds in the diet.
2. How do helminths affect the mental health of infected individuals?
The article discusses physical symptoms and complications but does not explore the psychological effects, such as anxiety, depression, or cognitive impairment, which can be associated with chronic helminth infections.
3. Are there any natural remedies for treating helminth infections?
The article focuses on anthelmintic drugs and supportive care but does not cover any alternative or natural treatments that might be used to treat or alleviate symptoms of helminth infections.
4. How do helminth infections impact the immune system beyond infection?
While the article mentions that helminths can modulate the host’s immune response, it does not detail how these infections might affect the immune system’s ability to respond to other diseases, vaccines, or allergens.
5. What is the economic impact of helminth infections on communities?
The article discusses the health implications of helminth infections but does not address their economic impact, such as reduced productivity, healthcare costs, and impacts on education and labor.
6. Are some people more susceptible to helminth infections than others?
The article does not explore factors that may make certain individuals more susceptible to helminth infections, such as genetic predisposition, existing health conditions, or specific environmental factors.
7. Can helminth infections affect pregnancy and childbirth?
While the article mentions maternal infections increasing the risk for early childhood infections, it does not provide specific details on how helminth infections might affect pregnancy outcomes, fetal development, or childbirth.
8. What are the global trends in helminth infections, and are they increasing or decreasing?
The article provides prevalence information but does not discuss current global trends, such as whether helminth infections are becoming more or less common in various regions or how climate change might affect these trends.
9. What is the role of animal reservoirs in human helminth infections?
The article touches on zoonotic potential but does not elaborate on the role that specific animal species play in maintaining and transmitting helminths to humans, or how these reservoirs might be controlled.
10. How does climate and environmental change influence helminth transmission?
The article briefly mentions climate affecting transmission patterns but does not delve into how specific changes, like increased rainfall, deforestation, or urbanization, might influence the spread and severity of helminth infections.