Alopecia areata (AA) is a common autoimmune disease characterized by non-scarring hair loss that can range from small patches on the scalp to complete hair loss across the entire body. The condition arises when the immune system mistakenly attacks hair follicles, leading to hair shedding. This autoimmune response is often associated with a collapse of immune privilege in the hair follicle, resulting in an inflammatory environment dominated by specific cytokines such as interferon-γ (IFNγ) and common gamma chain (γc) cytokines like IL-2, IL-7, and IL-15. AA can be triggered by genetic, immunological, endocrine, or psychological factors and is sometimes linked with other autoimmune diseases such as thyroid disorders and vitiligo. Diagnosis may involve a scalp biopsy, and treatment options include corticosteroids, topical minoxidil, and emerging therapies like Janus kinase (JAK) inhibitors, which have shown promise in clinical trials for promoting hair regrowth.
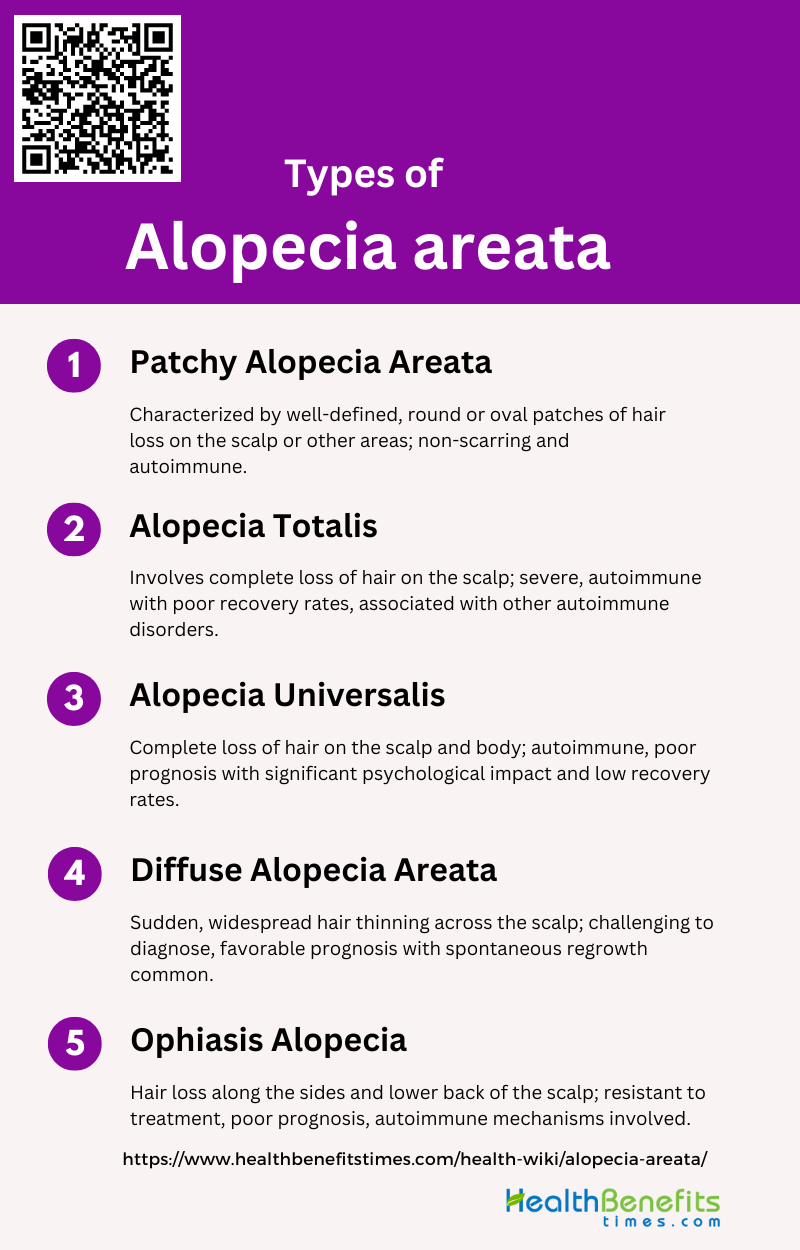
Types of Alopecia areata
Understanding the different types can help in recognizing and managing the condition effectively. Below are the main types of alopecia areata:
1. Patchy Alopecia Areata
Patchy alopecia areata is the most common form of alopecia areata, characterized by well-defined, round or oval patches of hair loss on the scalp or other hair-bearing areas of the body. This type of alopecia is non-scarring, meaning the hair follicles remain intact and have the potential to regrow hair. The condition is believed to be autoimmune in nature, with CD8+NKG2D+ T cells playing a significant role in the pathogenesis by attacking the hair follicles. Patchy alopecia areata can be diagnosed through clinical examination, dermoscopy, and sometimes histopathology, which reveals a lymphocytic infiltrate around the hair follicles. The prevalence of alopecia areata, including its patchy form, is approximately 2% globally.
2. Alopecia Totalis
Alopecia totalis is a more severe form of alopecia areata, characterized by the complete loss of hair on the scalp. This condition can be particularly distressing for patients due to its dramatic appearance and the psychological impact of total hair loss. The pathogenesis involves autoimmune mechanisms similar to those in patchy alopecia areata, with lymphocytic infiltrations and the presence of IFN-γ and IgG antibodies against hair follicle cells. Long-term outcomes for alopecia totalis are generally poor, with only a small percentage of patients achieving complete recovery. The condition is often associated with other autoimmune disorders, such as thyroid disease and vitiligo.
3. Alopecia Universalis
Alopecia universalis is the most severe form of alopecia areata, involving the complete loss of hair on the scalp and body, including eyebrows, eyelashes, and other body hair. Like alopecia totalis, it is an autoimmune condition where the body’s immune system attacks hair follicles, leading to widespread hair loss. The prognosis for alopecia universalis is generally unfavorable, with low rates of complete recovery and a high likelihood of psychological distress due to the extensive hair loss. The condition is often associated with other autoimmune diseases and can significantly impact the quality of life.
4. Diffuse Alopecia Areata
Diffuse alopecia areata is characterized by a sudden and widespread thinning of hair across the scalp, rather than well-defined patches. This form of alopecia areata can be challenging to diagnose due to its resemblance to other types of diffuse hair loss, such as telogen effluvium. Histopathological examination typically shows mononuclear cell infiltration around hair follicles and pigment incontinence. Despite its alarming presentation, diffuse alopecia areata often has a favorable prognosis, with many patients experiencing spontaneous hair regrowth within a few months, even without treatment.
5. Ophiasis Alopecia
Ophiasis alopecia is a unique pattern of alopecia areata characterized by hair loss along the sides and lower back of the scalp, resembling a snake-like shape. This form of alopecia is often more resistant to treatment and has a poorer prognosis compared to other types of alopecia areata. The autoimmune mechanisms underlying ophiasis alopecia are similar to those in other forms of alopecia areata, involving lymphocytic infiltrations and immune privilege breakdown of hair follicles. The prevalence of ophiasis alopecia is relatively low, and it is often associated with more severe and long-lasting cases of alopecia areata.
Causes and Risk Factors of Alopecia areata
Understanding these factors is crucial for better management and treatment of the disease. Below are some of the primary causes and risk factors associated with alopecia areata:
1. Genetic Predispositions
Genetic susceptibility plays a significant role in the development of AA, as evidenced by the association with other autoimmune conditions such as thyroiditis and vitiligo. Genome-wide association studies have identified several genetic loci linked to AA, suggesting a hereditary component. Additionally, the presence of AA in family members increases the likelihood of developing the condition, indicating a strong genetic predisposition.
2. Environmental Triggers
Environmental factors are crucial in the pathogenesis of AA. Psychological stress is a well-known trigger, but other environmental stimuli such as smoking, alcohol consumption, sleep patterns, obesity, and dietary factors like fatty acids and gluten consumption also play a role. These factors can exacerbate the inflammatory response in the hair follicles, leading to hair loss. The interplay between genetic predisposition and environmental triggers is complex and requires further investigation to fully understand their combined impact on AA.
3. Seasonal Allergies
Seasonal allergies, particularly allergic rhinitis, have been associated with an increased risk of developing AA. Studies have shown that patients with AA often have a higher prevalence of atopic conditions, including allergic rhinitis, asthma, and atopic dermatitis. The inflammatory response triggered by seasonal allergens may contribute to the autoimmune attack on hair follicles, exacerbating hair loss in susceptible individuals.
4. Thyroid Disease
Thyroid dysfunction, particularly autoimmune thyroid diseases like Hashimoto’s thyroiditis and Graves’ disease, is strongly associated with AA. Patients with AA have a higher prevalence of thyroid disorders, and the risk increases with age. The autoimmune nature of both conditions suggests a shared pathophysiological mechanism, where the immune system mistakenly targets both the thyroid gland and hair follicles.
5. Vitiligo
Vitiligo, an autoimmune condition characterized by the loss of skin pigmentation, is frequently associated with AA. Both conditions share common genetic and immunological pathways, and patients with AA are at a higher risk of developing vitiligo. The co-occurrence of these conditions suggests a broader autoimmune predisposition, where the immune system targets multiple tissues, including hair follicles and melanocytes.
6. Certain Health Conditions
AA is associated with various systemic diseases, including autoimmune disorders like lupus erythematosus, rheumatoid arthritis, and psoriasis. Patients with AA are also at an increased risk of developing psychiatric conditions such as depression and anxiety, which can further impact their quality of life. The presence of these comorbidities highlights the need for a comprehensive approach to managing AA, addressing both the physical and psychological aspects of the disease.
7. Vitamin and Mineral Deficiencies
Deficiencies in micronutrients such as vitamin D, zinc, and folate have been implicated in the development of AA. These nutrients play essential roles in immune function and hair follicle health, and their deficiency may exacerbate the autoimmune response in AA. While current evidence is not conclusive, supplementation of these micronutrients could offer a low-risk therapeutic option for managing AA, either as a primary treatment or as an adjunct to other therapies.
8. Age
The age of onset of AA can influence the disease’s progression and associated comorbidities. AA can occur at any age, but the first onset is most common in the third and fourth decades of life. An earlier age of onset is associated with a higher lifetime risk of extensive disease and a greater likelihood of developing other autoimmune conditions. Understanding the age-related patterns of AA can help clinicians tailor their management strategies to the specific needs of different age groups.
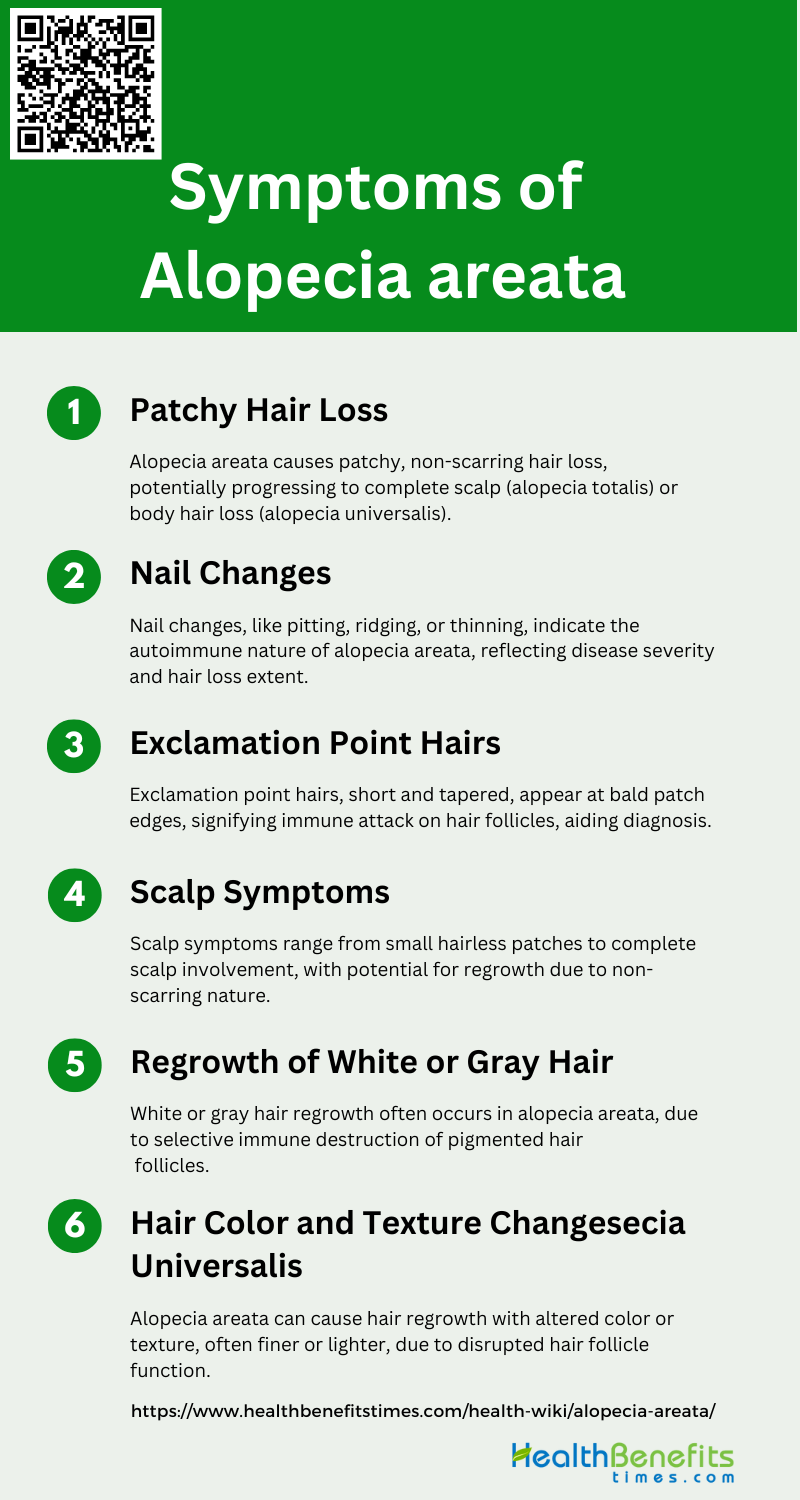
Symptoms of Alopecia areata
The symptoms can vary from person to person, but some common indicators are often observed. Here are some of the primary symptoms to look out for:
1. Patchy Hair Loss
Alopecia areata (AA) is primarily characterized by patchy hair loss, which can progress to more extensive forms such as alopecia totalis (complete scalp hair loss) or alopecia universalis (total body hair loss). The condition is autoimmune in nature, with CD8+NKG2D+ T cells playing a significant role in the pathogenesis by targeting hair follicles. The hair loss is typically non-scarring and can affect any hair-bearing area of the body, although the scalp is most commonly involved. The unpredictable nature of AA can be psychologically distressing for patients, contributing to anxiety and depression.
2. Nail Changes
Nail changes are a common manifestation in patients with alopecia areata, often presenting as nail pitting, ridging, or thinning. These changes are indicative of the autoimmune nature of the disease, as the same immune mechanisms that target hair follicles can also affect nail matrices. The presence of nail dystrophy can be a marker of disease severity and may correlate with more extensive hair loss. JAK inhibitors have shown promise in reversing nail dystrophy in patients with refractory AA, highlighting the potential for targeted therapies to address both hair and nail symptoms.
3. Exclamation Point Hairs
Exclamation point hairs are a hallmark of alopecia areata and are characterized by short, broken hairs that taper at the base, resembling an exclamation mark. These hairs are typically found at the periphery of bald patches and are a result of the immune-mediated attack on hair follicles, which weakens the hair shaft. Trichoscopy, a non-invasive diagnostic tool, can help identify these hairs and differentiate AA from other hair loss disorders. The presence of exclamation point hairs is a key diagnostic feature and can aid in the early detection and management of AA.
4. Scalp Symptoms
Scalp symptoms in alopecia areata can vary widely, ranging from small, well-circumscribed patches of hair loss to complete scalp involvement. The condition is non-scarring, meaning the hair follicles are preserved, which allows for the potential of hair regrowth. Inflammatory infiltrates, primarily composed of lymphocytes, are often observed around the hair follicles in affected areas. The breakdown of immune privilege in the hair follicle is believed to be a critical factor in the pathogenesis of AA, leading to localized inflammation and hair loss.
5. Regrowth of White or Gray Hair
Regrowth of white or gray hair is a phenomenon often observed in patients with alopecia areata, particularly during the early stages of hair regrowth. This can occur due to the selective destruction of pigmented hair follicles by the immune system, sparing non-pigmented (white or gray) hairs. Various forms of white hair regrowth have been documented, including transient and permanent white hair, as well as spearing of white hair in a patchy or diffuse pattern. The underlying mechanisms are thought to involve melanogenesis-associated molecules that trigger autoimmunity.
6. Hair Color and Texture Changes
Changes in hair color and texture are common in alopecia areata and can be indicative of the disease’s impact on hair follicle function. Patients may experience regrowth of hair that is different in color or texture from their original hair, often appearing finer or lighter. These changes are believed to result from the immune-mediated disruption of normal hair follicle cycling and melanogenesis. Understanding these alterations can provide insights into the pathophysiological mechanisms of AA and help in developing targeted therapies to restore normal hair growth.
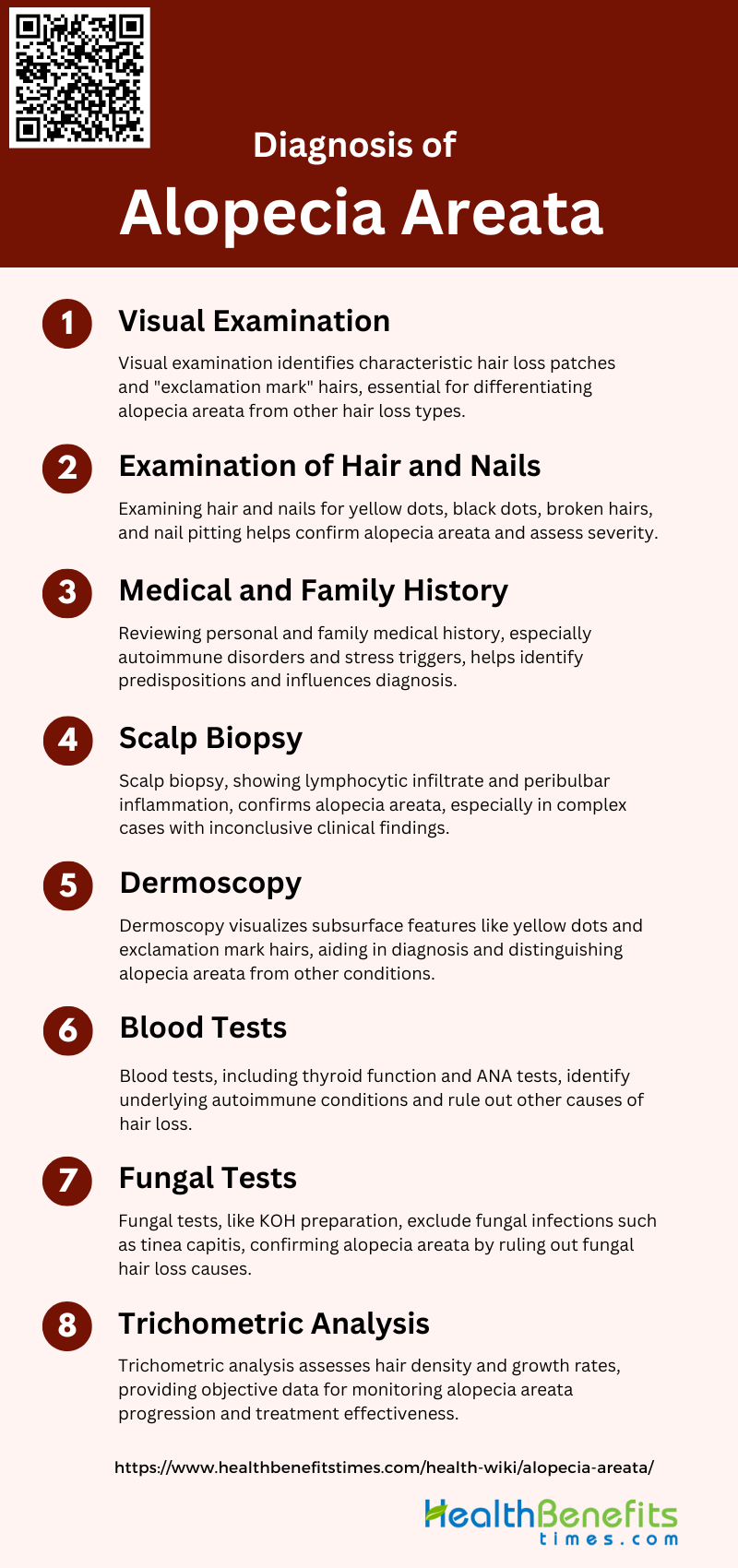
Diagnosis of Alopecia areata
Diagnosing Alopecia areata involves a thorough clinical examination and medical history review. Dermatologists often perform a scalp biopsy and blood tests to rule out other conditions. Here are the key steps involved in the diagnosis:
1. Visual Examination
Visual examination is the initial step in diagnosing alopecia areata, where clinicians look for characteristic signs such as well-defined patches of hair loss on the scalp or other hair-bearing areas. The presence of “exclamation mark” hairs, which are short broken hairs that taper at the base, is a hallmark of the condition. Additionally, the examination may reveal non-scarring, circular areas of hair loss with preserved follicular openings. This method is crucial for identifying the typical clinical manifestations of alopecia areata and differentiating it from other forms of hair loss.
2. Examination of Hair and Nails
A thorough examination of hair and nails is essential in diagnosing alopecia areata. Clinicians often observe the scalp for signs such as yellow dots, black dots, broken hairs, and short vellus hairs, which are indicative of the condition. Nail changes, such as pitting, trachyonychia, and longitudinal ridging, are also common in patients with alopecia areata and can provide additional diagnostic clues. These findings help in confirming the diagnosis and assessing the extent and activity of the disease.
3. Medical and Family History
Taking a detailed medical and family history is a critical component in diagnosing alopecia areata. Patients often have a personal or family history of autoimmune disorders such as vitiligo, thyroid disease, or atopic conditions. A history of recent stressful events or other triggers may also be relevant. Understanding the patient’s medical background helps in identifying potential genetic predispositions and comorbidities, this can influence the diagnosis and management of alopecia areata.
4. Scalp Biopsy
Scalp biopsy is a valuable diagnostic tool, especially in complex or atypical cases of alopecia areata. Histopathological examination of the biopsy specimen typically shows a lymphocytic infiltrate around the hair follicles, particularly in the anagen phase. This method can confirm the diagnosis by revealing characteristic features such as peribulbar inflammation and miniaturized hair follicles. Scalp biopsy is often used when clinical and dermoscopic findings are inconclusive.
5. Dermoscopy
Dermoscopy, also known as trichoscopy when applied to hair and scalp, is a non-invasive technique that enhances the visualization of subsurface features. It is particularly useful in identifying specific patterns such as yellow dots, black dots, broken hairs, and exclamation mark hairs, which are indicative of alopecia areata. Dermoscopy can also help in differentiating alopecia areata from other hair loss disorders and in assessing disease activity and severity.
6. Blood Tests
Blood tests are conducted to rule out other potential causes of hair loss and to identify any underlying autoimmune or systemic conditions. Common tests include thyroid function tests, antinuclear antibody (ANA) tests, and complete blood counts. These tests help in detecting associated autoimmune disorders such as thyroid disease, which is often seen in patients with alopecia areata. Blood tests provide a comprehensive understanding of the patient’s overall health and any contributing factors to hair loss.
7. Fungal Tests
Fungal tests, including KOH (potassium hydroxide) preparation and fungal cultures, are performed to exclude fungal infections such as tinea capitis, which can mimic alopecia areata. These tests involve taking samples from the affected scalp areas and examining them for fungal elements. Negative results help in confirming the diagnosis of alopecia areata by ruling out fungal causes of hair loss.
8. Trichometric Analysis
Trichometric analysis involves the quantitative assessment of hair density, hair diameter, and hair growth rate. This method provides objective data on the extent of hair loss and the effectiveness of treatment over time. Trichometric analysis can be performed using various tools and techniques, including phototrichograms and computerized hair analysis systems. This analysis is valuable for monitoring disease progression and response to therapy in patients with alopecia areata.
Treatment Options for Alopecia areata
Treating Alopecia areata involves various approaches depending on the severity and extent of hair loss. Dermatologists may recommend topical treatments, oral medications, or even light therapy. Here are some common treatment options:
1. Intralesional Corticosteroids
Intralesional corticosteroids are a common treatment for alopecia areata, showing significant efficacy in hair regrowth. Studies indicate that intralesional glucocorticosteroids have a high response rate, making them a preferred option for both adults and children with alopecia areata. However, they may have side effects and a high rate of relapse.
2. Minoxidil (Rogaine®)
Minoxidil is another widely used treatment for alopecia areata. It has been shown to be effective in promoting hair regrowth, particularly in patients with less than full scalp involvement. Studies comparing minoxidil to platelet-rich plasma (PRP) found that minoxidil resulted in significant increases in hair count and density, although PRP showed better quality of life improvements.
3. Phototherapy
Phototherapy, including ultraviolet radiation (UVR) and laser-based modalities, is emerging as a practical option for treating alopecia areata. Although there is strong potential for these treatments, high-quality evidence supporting their efficacy is still lacking, and more randomized control trials are needed.
4. Platelet-rich Plasma
Platelet-rich plasma (PRP) has shown promise in treating alopecia areata, with studies indicating significant hair regrowth and patient satisfaction. PRP can be administered via intradermal injection or enhanced transepidermal delivery methods like fractional CO2 laser or microneedling, which reduce pain and improve coverage.
5. Topical Immunotherapy
Topical immunotherapy, such as diphenylcyclopropenone (DPCP), has been used with variable success. It has shown a 38% success rate in producing cosmetically acceptable regrowth in patients with chronic severe alopecia areata. Combining DPCP with minoxidil did not show additional benefits.
6. Styling Techniques
Styling techniques are often used as a complementary approach to manage the appearance of hair loss. These techniques do not treat the underlying condition but can help improve the psychological well-being of patients by providing cosmetic solutions to mask hair loss.
7. Laser and Light Therapy
Laser and light therapy, including excimer laser and fractional CO2 laser, have been evaluated for their effectiveness in treating alopecia areata. These therapies show potential, especially when combined with other treatments like PRP, but more high-quality studies are needed to confirm their efficacy.
8. Immunosuppressants
Immunosuppressants, including systemic glucocorticosteroids and JAK inhibitors, have been considered effective in treating alopecia areata. These treatments are particularly useful in severe cases, although they come with potential side effects and require careful monitoring.
9. Cosmetic and Protective Techniques
Cosmetic and protective techniques, such as wigs, hairpieces, and scalp micropigmentation, provide non-medical options for managing alopecia areata. These methods help improve the appearance of hair loss and can significantly enhance the quality of life for patients.
Natural Treatment options for Alopecia areata
Exploring natural treatments for Alopecia areata can offer alternative solutions for those seeking holistic approaches. These methods may include dietary changes, essential oils, and stress management techniques. Here are some popular natural treatment options:
1. Acupuncture
Acupuncture, a traditional Chinese medicine practice, involves inserting needles into specific points on the body to stimulate healing and improve health. Recent studies suggest that acupuncture may be effective in treating alopecia areata by modulating the immune system and reducing inflammation. Targeted acupuncture points such as ST 36, GV 20, and LR 3 have shown promise in promoting hair regrowth. The treatment is generally well-tolerated with minimal side effects, making it a viable option for those seeking alternative therapies for hair loss.
2. Aromatherapy
Aromatherapy, which involves the use of essential oils, has been studied for its potential benefits in treating alopecia areata. A randomized controlled trial demonstrated that a blend of essential oils, including thyme, rosemary, lavender, and cedarwood, significantly improved hair regrowth in patients compared to a control group using only carrier oils. The study concluded that aromatherapy is a safe and effective treatment for alopecia areata, with a notable improvement in hair density and quality.
3. Vitamins and Supplements such as Zinc and Biotin
Vitamins and supplements, particularly zinc and biotin, are often recommended for improving hair health. Zinc plays a crucial role in hair tissue growth and repair, while biotin (vitamin B7) is essential for keratin production. Although there is limited direct evidence linking these supplements to the treatment of alopecia areata, their role in maintaining overall hair health makes them a popular choice among patients. Further research is needed to establish their efficacy in treating alopecia areata specifically.
4. Essential Oils
Essential oils such as peppermint, lavender, and rosemary have been explored for their potential benefits in treating alopecia areata. These oils are believed to improve blood circulation to the scalp, promote hair growth, and reduce inflammation. Clinical studies have shown that essential oils can be effective when used in combination with carrier oils for scalp massage, leading to significant hair regrowth in some patients.
5. Onion Juice
Onion juice has been studied as a topical treatment for alopecia areata. A clinical trial involving patients with patchy alopecia areata found that applying crude onion juice to the scalp twice daily resulted in significant hair regrowth. The study reported that 86.9% of patients experienced hair regrowth after six weeks of treatment, compared to only 13% in the control group using tap water. Onion juice is believed to stimulate hair follicles and improve blood circulation, making it an effective natural remedy for alopecia areata.
6. Probiotics
Probiotics, which are beneficial bacteria that support gut health, have been investigated for their potential role in treating autoimmune conditions, including alopecia areata. While direct evidence linking probiotics to hair regrowth in alopecia areata is limited, improving gut health can positively impact the immune system and reduce inflammation. This, in turn, may help manage autoimmune conditions and promote overall health, including hair health.
7. Healthy Diet
A healthy diet rich in vitamins, minerals, and antioxidants is essential for maintaining hair health and potentially managing alopecia areata. Nutrients such as vitamins A, C, D, E, zinc, and omega-3 fatty acids play a crucial role in hair growth and repair. A balanced diet that includes a variety of fruits, vegetables, lean proteins, and healthy fats can support the immune system and overall health, potentially reducing the severity of alopecia areata.
8. Stress Reduction Techniques
Stress reduction techniques such as mindfulness, meditation, yoga, and psychotherapy can be beneficial for managing alopecia areata. Stress is known to exacerbate autoimmune conditions, including alopecia areata. Techniques that reduce stress can help improve psychological well-being and potentially reduce the severity of hair loss. Studies have shown that therapies like hypnosis and mindfulness can improve the quality of life and psychological outcomes for patients with alopecia areata.
9. Herbal Supplements
Herbal supplements such as garlic, peony glucosides, and various botanical oils have been explored for their potential benefits in treating alopecia areata. Garlic supplements, for example, have shown promise in promoting hair regrowth due to their anti-inflammatory and antimicrobial properties. Other herbal ingredients like peony glucosides have been studied for their immunomodulatory effects, which can help manage autoimmune conditions like alopecia areata.
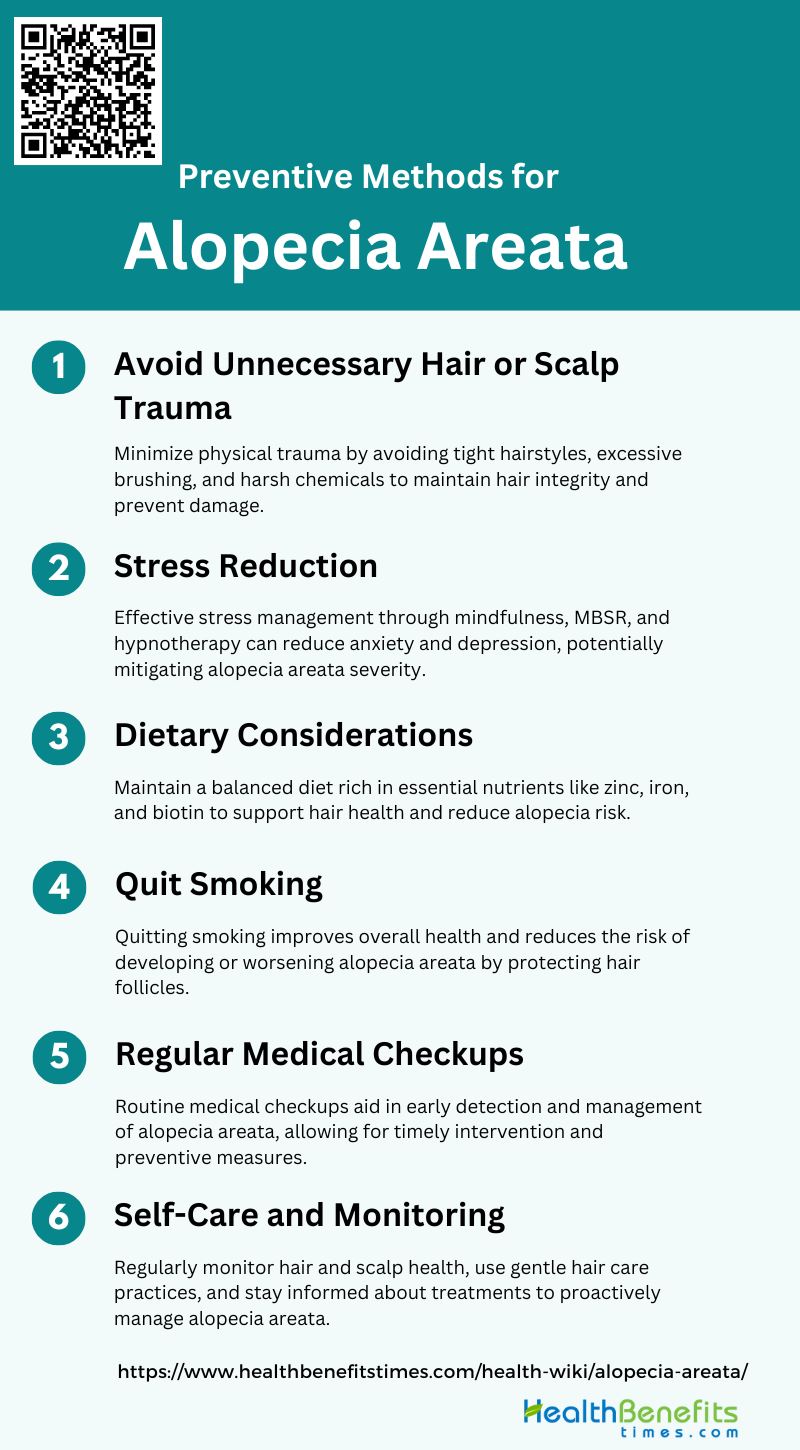
Preventive methods for Alopecia areata
Preventing Alopecia areata can be challenging, but certain lifestyle changes and practices may help reduce the risk. These methods include maintaining a healthy diet, managing stress, and avoiding harsh hair treatments. Here are some effective preventive measures:
1. Avoid Unnecessary Hair or Scalp Trauma
Minimizing physical trauma to the hair and scalp is crucial in preventing alopecia areata. Traumatic practices such as tight hairstyles, excessive brushing, and harsh chemical treatments can exacerbate hair loss. Studies have shown that reducing mechanical stress on hair follicles can help maintain hair integrity and prevent further damage. Additionally, avoiding unnecessary scalp trauma can reduce inflammation and the risk of triggering autoimmune responses that contribute to alopecia areata.
2. Stress Reduction
Stress is a significant factor in the onset and progression of alopecia areata. Psychological interventions, such as mindfulness-based stress reduction (MBSR) and hypnotherapy, have been shown to improve mental health and potentially promote hair regrowth. These interventions help reduce anxiety, depression, and other stress-related symptoms, which are often associated with hair loss. By managing stress effectively, individuals can potentially mitigate the severity of alopecia areata and improve their overall quality of life.
3. Dietary Considerations
A balanced diet rich in essential nutrients can play a vital role in preventing alopecia areata. Nutritional deficiencies, particularly in vitamins and minerals such as zinc, iron, and biotin, have been linked to hair loss. Ensuring adequate intake of these nutrients through a well-rounded diet or supplements can support hair health and potentially reduce the risk of alopecia areata. Additionally, some studies suggest that certain dietary modifications, such as reducing inflammatory foods, may help manage autoimmune conditions.
4. Quit Smoking
Smoking has been identified as a risk factor for various autoimmune diseases, including alopecia areata. The harmful chemicals in tobacco smoke can damage hair follicles and exacerbate hair loss. Quitting smoking can improve overall health and reduce the risk of developing or worsening alopecia areata. By eliminating this harmful habit, individuals can support their immune system and promote healthier hair growth.
5. Regular Medical Checkups
Regular medical checkups are essential for early detection and management of alopecia areata. Routine visits to a healthcare provider can help monitor hair health and identify any underlying conditions that may contribute to hair loss. Early intervention with appropriate treatments, such as corticosteroids or JAK inhibitors, can improve outcomes and potentially prevent severe hair loss. Regular checkups also provide an opportunity to discuss preventive measures and receive personalized advice from medical professionals6.
6. Self-Care and Monitoring
Self-care and regular monitoring of hair and scalp health are important preventive measures for alopecia areata. Individuals should be vigilant about changes in their hair density and seek medical advice if they notice unusual hair loss patterns. Implementing a gentle hair care routine, using mild shampoos, and avoiding excessive heat styling can help maintain hair health. Additionally, staying informed about the latest research and treatment options can empower individuals to take proactive steps in managing their condition.