 Alpha-1 Antitrypsin Deficiency (AATD) is a common autosomal recessive genetic disorder caused by mutations in the SERPINA1 gene, leading to the production of misfolded alpha-1 antitrypsin (AAT) protein. This glycoprotein, primarily produced in the liver, belongs to the serine protease inhibitor family and plays a crucial role in protecting tissues from enzyme damage, particularly in the lungs. The deficiency results in reduced levels of functional AAT in the bloodstream, causing uncontrolled activity of proteolytic enzymes like elastase, which can lead to the destruction of connective tissue, especially in the lungs, resulting in conditions such as pulmonary emphysema. Additionally, the accumulation of misfolded AAT in the liver can cause liver diseases, including cirrhosis and hepatocellular carcinoma. AATD is often underdiagnosed and can present with a variety of symptoms affecting multiple organs, necessitating comprehensive management and monitoring.
Alpha-1 Antitrypsin Deficiency (AATD) is a common autosomal recessive genetic disorder caused by mutations in the SERPINA1 gene, leading to the production of misfolded alpha-1 antitrypsin (AAT) protein. This glycoprotein, primarily produced in the liver, belongs to the serine protease inhibitor family and plays a crucial role in protecting tissues from enzyme damage, particularly in the lungs. The deficiency results in reduced levels of functional AAT in the bloodstream, causing uncontrolled activity of proteolytic enzymes like elastase, which can lead to the destruction of connective tissue, especially in the lungs, resulting in conditions such as pulmonary emphysema. Additionally, the accumulation of misfolded AAT in the liver can cause liver diseases, including cirrhosis and hepatocellular carcinoma. AATD is often underdiagnosed and can present with a variety of symptoms affecting multiple organs, necessitating comprehensive management and monitoring.
Overview of Alpha-1 Antitrypsin Deficiency
Who does Alpha-1 affect?
Alpha-1 antitrypsin deficiency (AATD) is a genetic disorder that primarily affects the lungs and liver, manifesting in both children and adults. It is characterized by low serum levels of alpha-1 antitrypsin (AAT), a protein that protects tissues from enzyme damage. The condition is most commonly associated with pulmonary emphysema and liver disease, with a higher prevalence in individuals of Northern European descent. Children with the ZZ-homozygous genotype are particularly affected, showing significant liver abnormalities and requiring long-term follow-up. Adults with AATD often experience chronic obstructive pulmonary disease (COPD) and may suffer from acute exacerbations, with a notable impact on their quality of life due to associated anxiety and depression. The prevalence of AATD varies, with estimates suggesting it affects between 1 in 1,600 to 1 in 6,000 individuals in Western Europe.
How common is Alpha-1?
The prevalence of the most common deficient genotype, PI*ZZ, is significant, with around 95% of individuals with severe AAT deficiency carrying this genotype. In the United States, the gene frequency of the M1 variant, a common form of AAT, is approximately 0.09. However, the prevalence of AAT deficiency varies globally. For instance, in Japan, AAT deficiency is considered rare, with only a few cases reported, predominantly involving the Siiyama variant. In contrast, a study in a southern Chinese population found that AAT deficiency is uncommon, with a very low frequency of deficiency variants. Despite the rarity of some variants, the so-called ‘rare’ AAT alleles may not be as rare as previously assumed, with studies suggesting a prevalence of around 1.6% for these alleles in certain populations. The establishment of patient registries, such as the one organized by the Alpha One Foundation, has facilitated the identification and study of individuals with AAT deficiency, further highlighting its prevalence and aiding in clinical research.
How does Alpha-1 deficiency affect my lungs and liver?
In the lungs, AATD leads to an increased risk of developing pulmonary emphysema, a progressive and irreversible lung disease characterized by the destruction of alveolar walls and loss of lung elasticity. This occurs because alpha-1 antitrypsin (AAT) is a protease inhibitor that normally protects the lungs from the damaging effects of neutrophil elastase, an enzyme that breaks down elastin in the lung tissue. When AAT levels are deficient, uninhibited neutrophil elastase can degrade the lung’s connective tissue matrix, leading to the development of emphysema, especially in individuals who smoke or are exposed to other environmental pollutants. In the liver, AATD can cause the accumulation of misfolded AAT proteins, leading to liver injury, cirrhosis, and in some cases, liver failure, particularly in children and adults.
Is Alpha-1 a terminal illness?
Alpha-1 antitrypsin deficiency is not necessarily a terminal illness, but it can lead to severe complications such as chronic obstructive pulmonary disease, cirrhosis, and hepatocellular carcinoma, which may result in premature death if untreated. Treatment options, including substitution therapy and organ transplantation, can manage symptoms and improve quality of life.
Symptoms and Causes
What are the symptoms of Alpha-1 antitrypsin deficiency?
The symptoms can vary widely among individuals and may appear at any age. Here are some common symptoms associated with this condition:
- Shortness of breath and wheezing: AATD can lead to the development of emphysema and chronic obstructive pulmonary disease (COPD), causing breathing difficulties and wheezing.
- Chronic cough: Patients with AATD-related lung disease often experience a persistent cough, which may be productive or dry.
- Recurrent respiratory infections: Individuals with AATD are more susceptible to respiratory infections, such as bronchitis and pneumonia, due to the lack of protective alpha-1 antitrypsin protein.
- Fatigue and decreased exercise tolerance: The lung damage caused by AATD can lead to fatigue and reduced ability to perform physical activities.
- Jaundice and liver disease: In some cases, particularly in children with severe AATD, the accumulation of abnormal alpha-1 antitrypsin protein in the liver can cause liver damage, leading to jaundice, abdominal swelling, and other signs of liver disease.
What causes Alpha-1 antitrypsin deficiency?
Alpha-1 antitrypsin deficiency (AATD) is primarily caused by genetic mutations that lead to the production of abnormal alpha-1 antitrypsin (AAT) proteins. These mutations often result in the accumulation of misfolded AAT proteins within the endoplasmic reticulum (ER) of hepatocytes, forming ordered polymers that cannot be secreted properly. This retention of mutant AAT in the liver cells can cause liver injury, including cirrhosis and hepatocellular carcinoma, particularly in a subset of individuals who may have additional genetic or environmental factors that exacerbate the condition. In the lungs, the deficiency of functional AAT allows for unchecked activity of neutrophil elastase, leading to the destruction of connective tissue and resulting in conditions such as emphysema and chronic obstructive pulmonary disease (COPD). Various mutations, including single base substitutions, deletions, or additions in the AAT gene, contribute to the deficiency, with some mutations leading to a complete lack of AAT production, known as “null” alleles.
Diagnosis and Tests
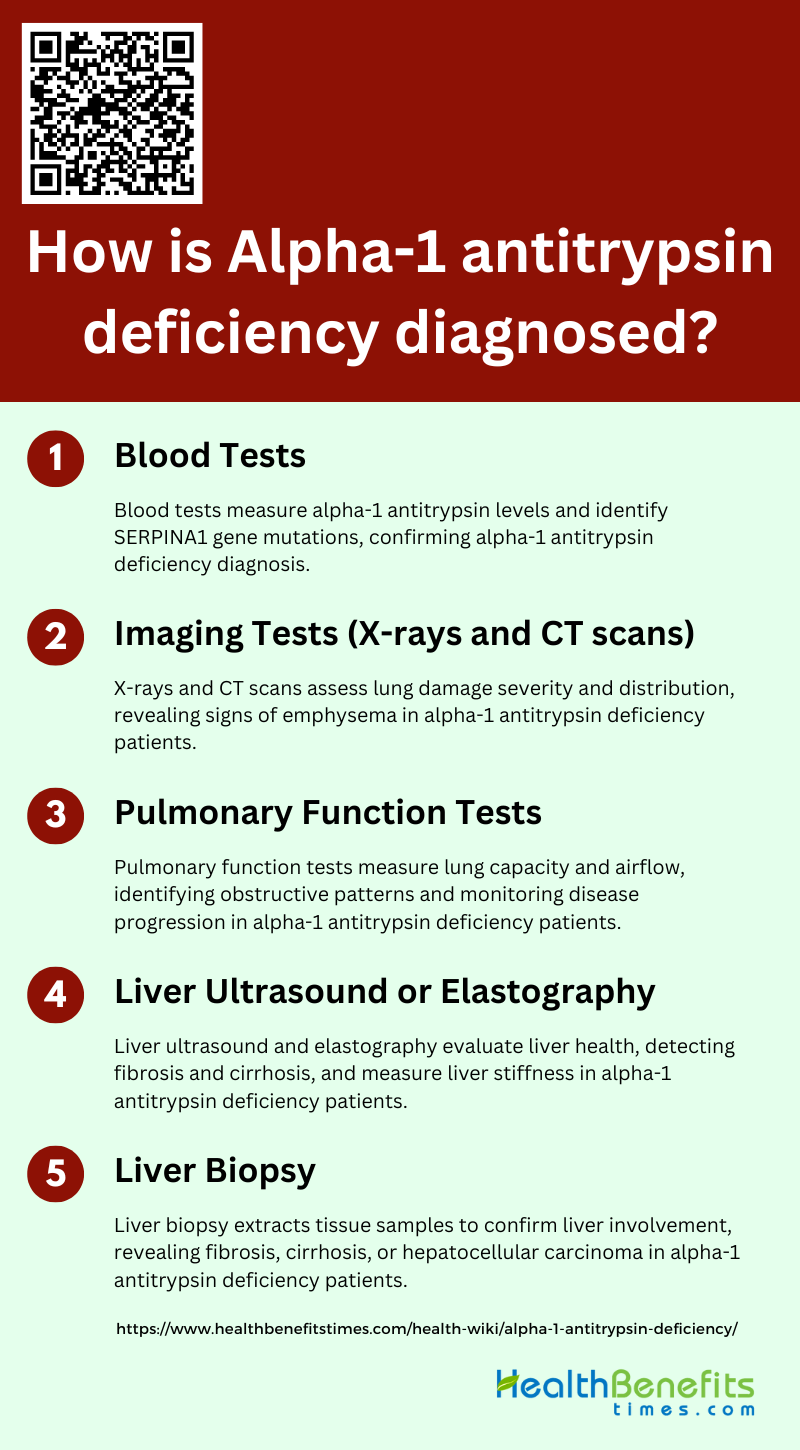
How is Alpha-1 antitrypsin deficiency diagnosed?
It is diagnosed through a combination of clinical evaluation, family history, and specific laboratory tests. These tests help determine the levels of alpha-1 antitrypsin in the blood and identify any genetic mutations. The following steps outline the diagnostic process:
1. Blood Tests
Low levels of AAT in the blood can indicate a deficiency. Genetic analysis can further confirm the diagnosis by identifying mutations in the SERPINA1 gene, which encodes the AAT protein. These tests are crucial for early detection and management of the disease, especially in individuals with a family history of AATD or related symptoms.
2. Imaging Tests (X-rays and CT scans)
Imaging tests such as X-rays and CT scans are used to assess the extent of lung damage in patients with AATD. These tests can reveal signs of emphysema, a common pulmonary manifestation of the deficiency. CT scans, in particular, provide detailed images that can help in evaluating the severity and distribution of lung damage, aiding in the diagnosis and monitoring of the disease progression.
3. Pulmonary Function Tests
Pulmonary function tests (PFTs) are essential in diagnosing and monitoring AATD. These tests measure lung capacity and airflow, helping to identify obstructive patterns typical of chronic obstructive pulmonary disease (COPD) and emphysema, which are common in AATD patients. A decreased FEV1/FVC ratio is often observed, indicating airflow obstruction and reduced lung function. Regular PFTs can help track disease progression and the effectiveness of treatments.
4. Liver Ultrasound or Elastography
Liver ultrasound and elastography are non-invasive imaging techniques used to evaluate liver health in AATD patients. These tests can detect liver abnormalities such as fibrosis and cirrhosis, which are potential complications of AATD. Elastography, in particular, measures liver stiffness, providing valuable information about the extent of liver damage and helping to guide further management and treatment.
5. Liver Biopsy
A liver biopsy may be performed to obtain a definitive diagnosis of liver involvement in AATD. This invasive procedure involves extracting a small sample of liver tissue for microscopic examination. It can reveal the presence of liver fibrosis, cirrhosis, or hepatocellular carcinoma, which are associated with AATD. Although not routinely performed, a liver biopsy is crucial for confirming the diagnosis and assessing the severity of liver disease in certain cases.
Management and Treatment
How is Alpha-1 treated?
Alpha-1 antitrypsin deficiency (AATD) is primarily treated through augmentation therapy, which involves the intravenous administration of alpha-1 antitrypsin (AAT) protein derived from pooled human plasma. This therapy aims to raise AAT levels in the blood and lung epithelial lining fluid, thereby increasing anti-elastase capacity and reducing inflammation in the lungs, which helps slow the progression of lung disease associated with AATD. Additionally, management of AATD includes lifestyle modifications such as avoiding environmental pollutants, improving exercise levels, and maintaining good nutritional status. For liver-related complications, non-invasive methods like liver stiffness measurement (LSM) via transient elastography are used to assess fibrosis, and liver transplantation may be considered in severe cases. Emerging treatments, including gene editing and chemical chaperones, are also under investigation to provide more effective and accessible options for AATD patients.
What medications/treatments are used?
Various medications and treatments are available to manage the symptoms and complications associated with AATD. Below is a list of commonly used treatments:
- Augmentation Therapy: Augmentation therapy involves the intravenous administration of exogenous alpha-1 antitrypsin (AAT) protein to patients with alpha-1 antitrypsin deficiency (AATD). This treatment raises AAT levels in the blood and lungs, enhancing anti-elastase capacity and reducing inflammation, thereby slowing the progression of emphysema and preserving lung function.
- Lifestyle Changes: Lifestyle changes are crucial in managing AATD. Patients are advised to avoid environmental pollutants, including tobacco smoke, and to improve their exercise levels and nutritional status. These changes help reduce the risk of lung infections and slow disease progression, improving overall health and quality of life.
- Medication: Medications for AATD primarily include bronchodilators and inhaled corticosteroids, which help manage symptoms of chronic obstructive pulmonary disease (COPD) associated with AATD. These medications alleviate breathing difficulties, reduce inflammation, and improve lung function, contributing to better disease management.
- Oxygen Therapy: Oxygen therapy is prescribed for AATD patients with severe lung disease who experience low blood oxygen levels. It helps maintain adequate oxygenation, reduces shortness of breath, and improves overall energy levels and quality of life, especially during physical activities and sleep.
- Pulmonary Rehabilitation: Pulmonary rehabilitation programs are designed to improve the physical and emotional well-being of AATD patients. These programs include exercise training, nutritional counseling, and education on managing lung disease, which collectively enhance lung function, reduce symptoms, and improve the patient’s ability to perform daily activities.
- Smoking Cessation Therapy: Smoking cessation therapy is critical for AATD patients, as smoking significantly accelerates lung damage. Therapies may include counseling, nicotine replacement products, and medications like varenicline or bupropion, which help patients quit smoking and reduce the risk of further lung deterioration.
- Lung Transplant: Lung transplantation is considered for AATD patients with end-stage lung disease who do not respond to other treatments. This procedure can significantly improve survival and quality of life by replacing the damaged lungs with healthy donor lungs, although it involves complex post-operative care and lifelong immunosuppression.
- Liver Transplant: Liver transplantation may be necessary for AATD patients who develop severe liver disease, such as cirrhosis. This procedure replaces the diseased liver with a healthy donor liver, potentially curing the liver-related aspects of AATD and significantly improving the patient’s prognosis and quality of life.
- Vaccinations: Vaccinations are essential for AATD patients to prevent respiratory infections, which can exacerbate lung disease. Recommended vaccines include influenza, pneumococcal, and hepatitis vaccines. These vaccinations help reduce the risk of severe infections and complications, thereby protecting lung and liver health.
What can’t I eat/drink with Alpha-1?
Individuals with Alpha-1 Antitrypsin Deficiency (AATD) should be cautious about their diet to manage their condition effectively. Alcohol consumption is particularly detrimental as it exacerbates liver damage, a common complication in AATD patients. High-fat diets and foods that increase cholesterol levels should also be avoided, as they can contribute to liver and cardiovascular issues. Additionally, smoking and exposure to environmental pollutants should be minimized, as they can worsen lung conditions associated with AATD. Therefore, a balanced diet low in alcohol, fats, and cholesterol, combined with a smoke-free lifestyle, is crucial for managing AATD.
Prevention
How can I prevent Alpha-1?
Preventing Alpha-1 Antitrypsin Deficiency involves a combination of lifestyle changes and medical interventions. Early diagnosis and proactive management are crucial in mitigating the effects of this genetic condition. Here are some steps you can take to prevent complications associated with Alpha-1
- Don’t smoke or vape: Avoiding smoking and vaping is crucial in preventing Alpha-1 Antitrypsin Deficiency (AATD) complications. Smoking accelerates lung damage and significantly increases the risk of developing chronic obstructive pulmonary disease (COPD) in individuals with AATD.
- Avoid lung irritants: Minimize exposure to lung irritants such as dust, fumes, and chemicals. Occupational exposure to these irritants can exacerbate lung function decline in individuals with AATD, leading to conditions like emphysema and chronic bronchitis.
- Avoid alcohol use: Limiting alcohol consumption is essential as it can exacerbate liver damage in individuals with AATD. Alcohol can increase the risk of liver disease progression, making it vital to avoid or minimize alcohol intake.
- Get vaccinated against infectious diseases: Vaccinations against influenza, pneumonia, and other infectious diseases are critical for individuals with AATD. These vaccinations help prevent respiratory infections that can worsen lung function and overall health.
- Regular Health Check-ups: Regular health check-ups are vital for early detection and management of AATD-related complications. Routine monitoring of lung and liver function can help manage the disease effectively and prevent severe outcomes.
- Healthy Lifestyle: Maintaining a healthy lifestyle, including a balanced diet and regular exercise, supports overall well-being and can mitigate the impact of AATD. Physical activity improves lung function and reduces the risk of comorbid conditions.
- Medications: Medications, including augmentation therapy, can help manage AATD by increasing the levels of alpha-1 antitrypsin in the blood. This therapy can slow disease progression and improve lung function, enhancing the quality of life.
Outlook / Prognosis
– What can I expect if I have Alpha-1? (1 paragraph)
What are the complications of Alpha-1?
Alpha-1 Antitrypsin Deficiency (Alpha-1) can lead to several complications, including:
- Emphysema: A severe lung condition characterized by damage to the air sacs (alveoli), leading to breathing difficulties and reduced oxygen exchange.
- Chronic Obstructive Pulmonary Disease (COPD): A progressive lung disease that includes chronic bronchitis and emphysema, causing long-term respiratory problems and decreased airflow.
- Liver Disease: Conditions such as cirrhosis and liver fibrosis can develop, leading to liver dysfunction and potentially liver failure. Hepatocellular carcinoma is also a risk.
- Panniculitis: A rare skin condition causing painful lumps or patches due to inflammation of the fat layer beneath the skin, which can occur in individuals with alpha-1 antitrypsin deficiency.
What is the life expectancy of someone with alpha-1 antitrypsin deficiency?
The life expectancy of individuals with alpha-1 antitrypsin deficiency (AATD) varies significantly based on the presence and severity of associated conditions, particularly lung and liver diseases. For those without chronic liver disease, life expectancy can be comparable to the general population. However, individuals with severe AATD, especially those with the PiZZ genotype, often develop emphysema and liver cirrhosis, which can significantly reduce life expectancy. Augmentation therapy with intravenous alpha-1 antitrypsin can slow the progression of lung disease and potentially extend survival, but its efficacy remains a subject of debate. Overall, the prognosis is highly individualized, depending on factors such as the severity of lung function decline, presence of liver disease, and response to treatments.
Living With
How do I take care of myself with Alpha-1?
Taking care of you with Alpha-1 Antitrypsin Deficiency (AATD) involves a combination of lifestyle changes, medical treatments, and regular monitoring. Key strategies include avoiding environmental pollutants such as tobacco smoke, which can exacerbate lung damage, and maintaining a healthy lifestyle through regular exercise and proper nutrition. Augmentation therapy, which involves weekly or biweekly intravenous infusions of alpha-1 antitrypsin protein, can help slow the progression of lung disease. Self-administration of this therapy at home can offer greater flexibility and improve quality of life. Regular check-ups with healthcare providers, including pulmonologists, and adherence to prescribed treatments are essential. Additionally, staying informed about your condition and participating in support programs can provide valuable resources and emotional support.
When should I see my healthcare provider?
It is crucial to consult your healthcare provider, especially your pulmonary specialist, if you notice an increase in coughing, mucus production, shortness of breath, wheezing, or chest tightness beyond your typical baseline. Seeking prompt medical evaluation and treatment for exacerbations can help prevent further lung damage and disease progression in AATD. Additionally, regular follow-up visits with your provider are essential for monitoring the condition, adjusting treatment plans, and discussing any concerns or questions you may have regarding your AATD management.
What questions should I ask my doctor?
- What symptoms should I watch for that might indicate a worsening of my condition?
- How often should I have follow-up appointments and tests to monitor my condition?
- How is AATD diagnosed, and what tests will I need to confirm the diagnosis?
- Should my family members be tested for AATD?
- What are the available treatment options for AATD, and which one do you recommend for me?
- Can you explain the benefits and risks of AAT augmentation therapy?
- Are there any new or experimental treatments available for AATD?
- What lifestyle changes can help manage my condition and improve my quality of life?
- Are there specific exercises or activities that are beneficial or should be avoided?