Postpartum cramping, also known as afterpains, refers to the contractions experienced by the uterus as it shrinks back to its pre-pregnancy size after giving birth. These cramps are caused by the uterine muscles tightening and relaxing to help expel any remaining blood and tissue from the uterus. The cramping is usually most intense within the first few days after delivery, particularly during breastfeeding when the hormone oxytocin triggers uterine contractions. While uncomfortable, these afterpains are a normal part of the postpartum recovery process and help reduce bleeding by compressing the blood vessels in the uterus.
Postpartum cramping, also known as afterpains, refers to the contractions experienced by the uterus as it shrinks back to its pre-pregnancy size after giving birth. These cramps are caused by the uterine muscles tightening and relaxing to help expel any remaining blood and tissue from the uterus. The cramping is usually most intense within the first few days after delivery, particularly during breastfeeding when the hormone oxytocin triggers uterine contractions. While uncomfortable, these afterpains are a normal part of the postpartum recovery process and help reduce bleeding by compressing the blood vessels in the uterus.
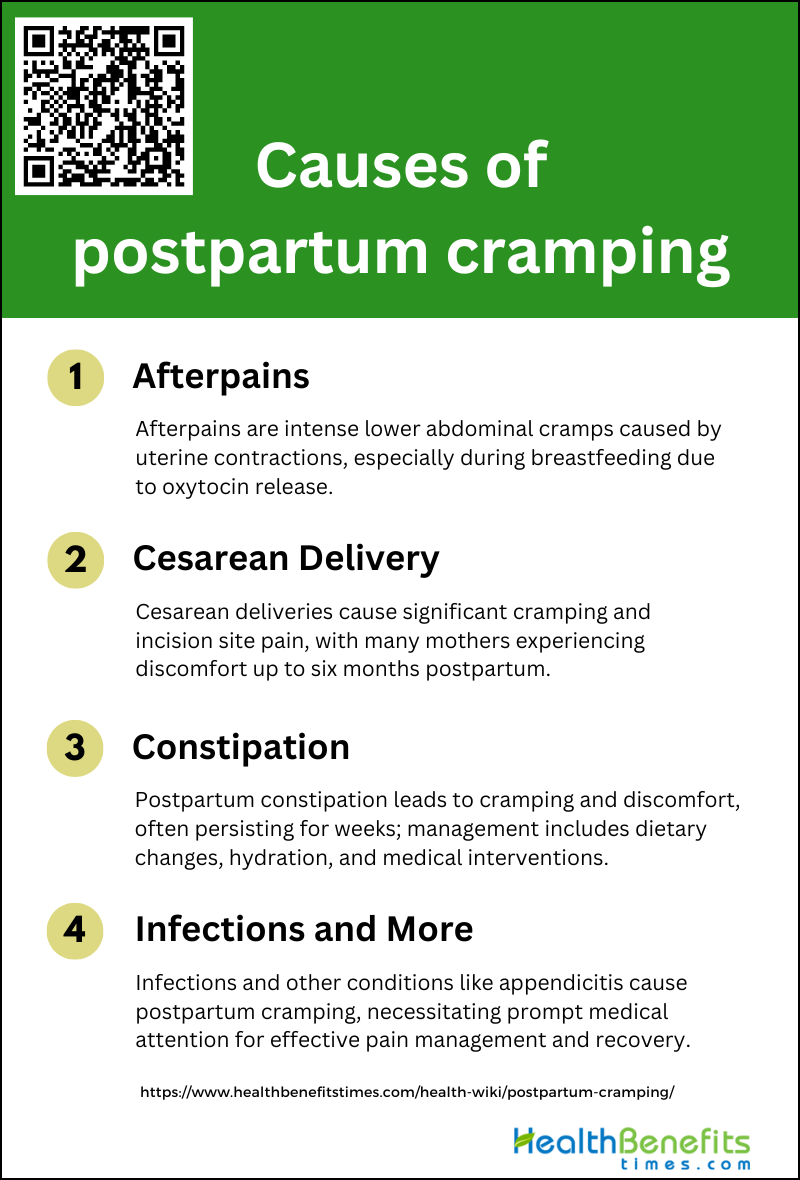
Causes of postpartum cramping
Postpartum cramps can range from mild to intense and are particularly common during breastfeeding. Below is a list of factors that contribute to postpartum cramping.
1. Afterpains
Afterpains are a common cause of postpartum cramping, characterized by lower abdominal pain due to prolonged uterine contractions. These contractions are particularly noticeable during breastfeeding, as the hormone oxytocin, which stimulates milk ejection, also causes the uterus to contract. The intensity of afterpains can be as severe as labor pains, making them a significant source of discomfort for new mothers. Effective pain management strategies are essential to address this issue, as postpartum pain thresholds tend to decrease, highlighting the need for specialized care from anesthesiologists and physical health therapists.
2. Cesarean Delivery
Cesarean delivery is another major cause of postpartum cramping and pain. According to a national survey, 79% of mothers who underwent a cesarean section reported experiencing pain at the incision site within the first two months postpartum. This pain was described as a major problem by 33% of these mothers, with 18% reporting that the pain persisted into the sixth month postpartum. The study also found that mothers with planned cesareans without labor were just as likely to report postpartum pain as those who had cesareans with labor. This highlights the need for effective pain management and support for mothers recovering from cesarean deliveries.
3. Constipation
Constipation is a common postpartum issue that can lead to significant cramping and discomfort. In a prospective cohort study, constipation was identified as one of the prevalent maternal physical health symptoms in the first eight weeks postpartum. The study found that birth-related pain, including constipation, was common, with many women experiencing persistent symptoms. Effective management of constipation through dietary adjustments, hydration, and possibly medical interventions is crucial to alleviate this source of postpartum cramping.
4. Infections and More
Postpartum infections, such as genital infections, can also cause significant cramping and pain. These infections are direct complications of parturition and require prompt medical attention to prevent further complications. Other potential causes of postpartum cramping include conditions like appendicitis, which, although fortuitous, can occur during the postpartum period. The focus on pain control during pregnancy often overlooks the postpartum period, necessitating a more comprehensive approach to managing postpartum pain and cramping. Early identification and treatment of these conditions are essential to ensure the well-being of new mothers.
Sign and symptoms of postpartum cramping
After giving birth, many new mothers experience postpartum cramping as their uterus contracts and shrinks back to its pre-pregnancy size. These cramps often referred to as “afterpains,” can vary in intensity and duration. The following are some common signs and symptoms:
- Vaginal bleeding
- Cramping
- Pain in your back, neck, or joints
- Pain in your perineum (the area between your vagina and anus)
- Pain around your incision (if you had a cesarean birth)
- Swollen breasts
- Bladder problems
- Bowel problems
- Hemorrhoids
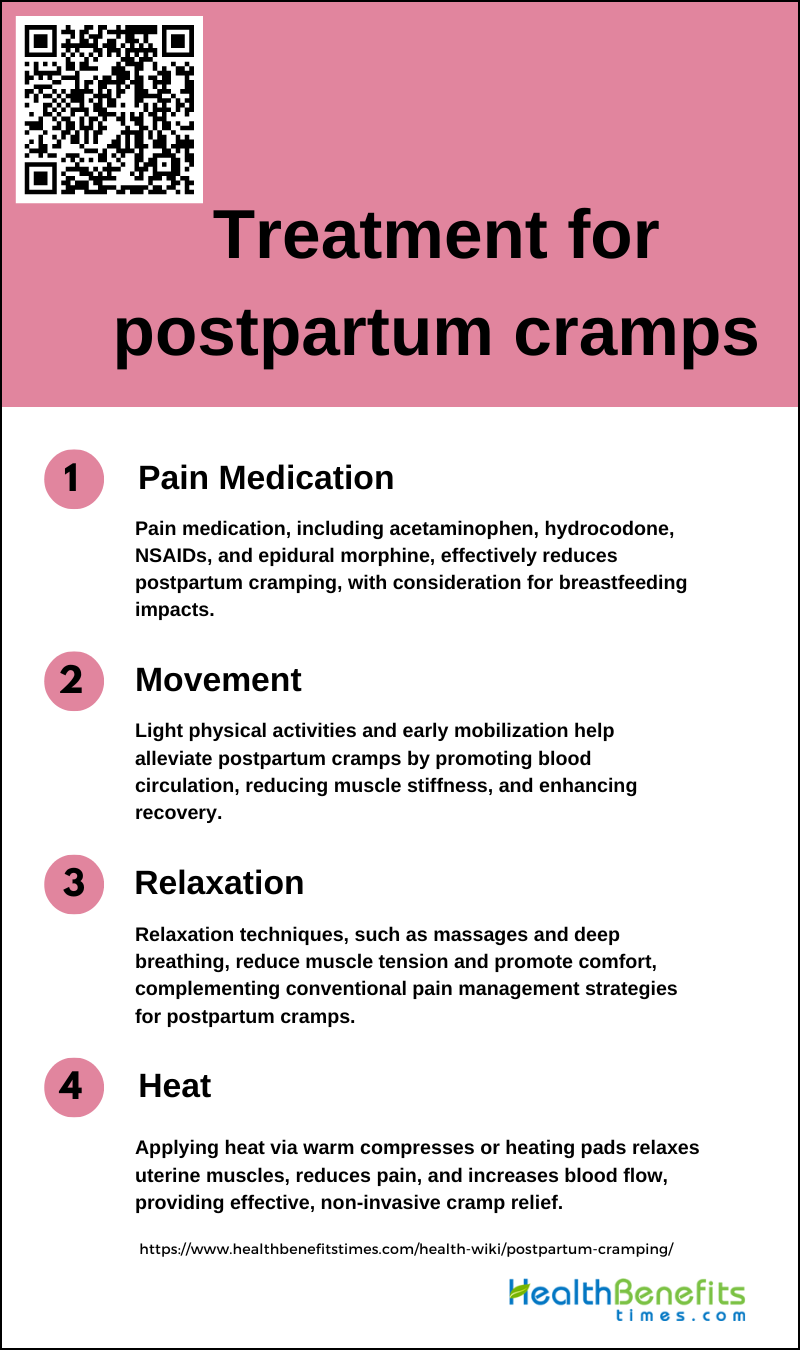
Treatment for postpartum cramps
Experiencing postpartum cramps is a common occurrence for new mothers as the uterus contracts back to its pre-pregnancy size. These cramps, often referred to as afterpains, can be uncomfortable but are a natural part of the healing process. Below is a list of treatments that can help alleviate the discomfort associated with postpartum cramps.
1. Pain Medication
Pain medication is a cornerstone in managing postpartum cramps. Various studies have demonstrated the efficacy of different analgesics. For instance, a combination of acetaminophen and hydrocodone has been shown to be significantly effective in reducing postpartum pain compared to placebo, with each component contributing to the overall analgesic effect through different mechanisms. Non-steroidal anti-inflammatory drugs (NSAIDs) like flurbiprofen and aspirin have also been found to provide substantial pain relief, often outperforming codeine in terms of efficacy and side effects. Additionally, a single dose of epidural morphine can significantly reduce the need for oral pain medication in the first 24 hours postpartum, offering a viable alternative for immediate pain management. However, it is crucial to consider the potential side effects and the impact on breastfeeding when prescribing these medications.
2. Movement
Movement and early mobilization are essential in managing postpartum cramps. Engaging in light physical activities such as postpartum gymnastics can help alleviate pain by promoting blood circulation and reducing muscle stiffness. Early mobilization has been associated with quicker recovery and reduced pain intensity, as it helps in the natural contraction and relaxation of the uterus, thereby easing cramps. Additionally, maintaining an active lifestyle postpartum can contribute to overall well-being and faster recovery of the reproductive organs to their pre-pregnancy state. Encouraging new mothers to engage in gentle exercises and providing guidance on safe movements can be beneficial in managing postpartum cramps effectively.
3. Relaxation
Relaxation techniques play a significant role in managing postpartum cramps. Methods like effleurage massage, sacral plexus massage, and candle therapy have been found to be effective in providing relief from afterpain. These techniques help in reducing muscle tension and promoting relaxation, which can alleviate the discomfort associated with uterine contractions. Additionally, creating a comfortable environment, ensuring adequate rest, and practicing relaxation techniques like deep breathing can further enhance pain relief. Complementary therapies, when combined with conventional pain management strategies, can offer a holistic approach to managing postpartum cramps, improving both physical and psychological well-being.
4. Heat
Applying heat is a simple yet effective method for managing postpartum cramps. Heat therapy, like using warm compresses or heating pads, can help relax the uterine muscles and reduce pain. The application of heat increases blood flow to the affected area, which can alleviate muscle spasms and provide comfort. This method is particularly beneficial as it is non-invasive and can be easily administered at home. Encouraging postpartum women to use heat therapy, along with other pain management strategies, can significantly improve their comfort and aid in the recovery process. Combining heat application with other relaxation techniques can further enhance its effectiveness in managing postpartum cramps.
When to seek medical advice for postpartum cramping
Postpartum cramping is a natural part of the healing process as your uterus returns to its pre-pregnancy size. But, certain symptoms can signal the need for medical attention. If you experience any of the following, it’s important to consult your healthcare provider promptly.
1 .Fever: If you have a fever of 100.4°F (38°C) or higher after giving birth, it could indicate an infection, so seek medical attention immediately.
2. Discharge: Unusual colored or foul-smelling vaginal discharge may signify an infection like endometritis or bacterial vaginosis, requiring prompt treatment.
3. Very heavy bleeding: Soaking through more than one pad every 1-2 hours or passing large clots could mean postpartum hemorrhage. Contact your doctor right away.
4. Painful urination: Frequent or painful urination after delivery may be a sign of a urinary tract infection (UTI) that needs antibiotic treatment to prevent complications.
5. Significant cramping or abdominal pain: While some cramping is normal, severe or persistent abdominal pain could indicate postpartum endometritis or other issues requiring medical evaluation.
6. Redness around incision: Redness, warmth, discharge or increasing pain around a C-section incision may signal an infection that needs treatment.
7. Severe headaches: A severe headache can be a symptom of postpartum preeclampsia, a serious condition requiring emergency medical care.
8. Complications with tears or incisions: Fever, foul odor, or worsening pain from vaginal tears or surgical incisions may mean an infection has developed.
9. Incontinence: Leaking urine, gas or bowel movements after delivery could indicate pelvic floor issues needing evaluation and therapy.
10. Frequent peeing or burning: While some discomfort is normal, severe burning or constant urge to urinate may signal a UTI.
11. Leg pain: Leg pain or swelling can sometimes indicate a blood clot, which requires urgent treatment.
12. Chest pain or trouble breathing: Shortness of breath or chest pain after delivery is concerning symptoms that should be evaluated promptly.
13. Breast pain or burning: While engorgement is common with milk production, severe breast pain, redness or burning warrants medical attention for potential infection.