Adrenal tumors are abnormal growths that develop in the adrenal glands, which are small hormone-producing glands located on top of the kidneys. These tumors can be either benign (non-cancerous) or malignant (cancerous). Benign adrenal tumors, such as adenomas, are the most common type and may or may not produce excess hormones. Malignant adrenal tumors, like adrenocortical carcinoma, are rare but aggressive cancers that can spread to other parts of the body and often overproduce hormones, leading to various symptoms. Adrenal tumors can also result from the metastasis (spread) of cancers from other organs, such as the lungs or breasts.
Adrenal tumors are abnormal growths that develop in the adrenal glands, which are small hormone-producing glands located on top of the kidneys. These tumors can be either benign (non-cancerous) or malignant (cancerous). Benign adrenal tumors, such as adenomas, are the most common type and may or may not produce excess hormones. Malignant adrenal tumors, like adrenocortical carcinoma, are rare but aggressive cancers that can spread to other parts of the body and often overproduce hormones, leading to various symptoms. Adrenal tumors can also result from the metastasis (spread) of cancers from other organs, such as the lungs or breasts.
Types of Adrenal Tumors
Below include types of adrenal tumors that medical professionals have identified.
1. Adrenal Cortex Tumors
Adrenal cortex tumors can be either benign or malignant. Benign tumors, like cortical adenomas, are often asymptomatic and typically discovered incidentally during autopsies or imaging for other conditions. Malignant tumors, like adrenocortical carcinomas, are more aggressive and can cause a variety of symptoms depending on the hormones they secrete. In children, these tumors can lead to precocious puberty and virilization, while in adults; they may cause Cushing’s syndrome, characterized by symptoms like plethoric adiposity, hypertension, and osteoporosis. The prognosis for malignant adrenal cortex tumors is generally poor, and surgical exploration is often necessary to confirm the diagnosis.
2. Adrenal Medulla Tumors
Adrenal medulla tumors, primarily pheochromocytomas, are usually benign but can cause significant clinical symptoms due to excessive catecholamine secretions. These symptoms include paroxysmal hypertension, tachycardia, sweating, nausea, and headaches. Pheochromocytomas can be part of composite tumors that include other cell types, such as ganglioneuromas, which further complicate their diagnosis and treatment. Despite their benign nature, the excessive hormone production can lead to severe cardiovascular complications if not managed properly. Surgical removal of these tumors generally results in favorable outcomes, provided there is no significant cardiovascular damage.
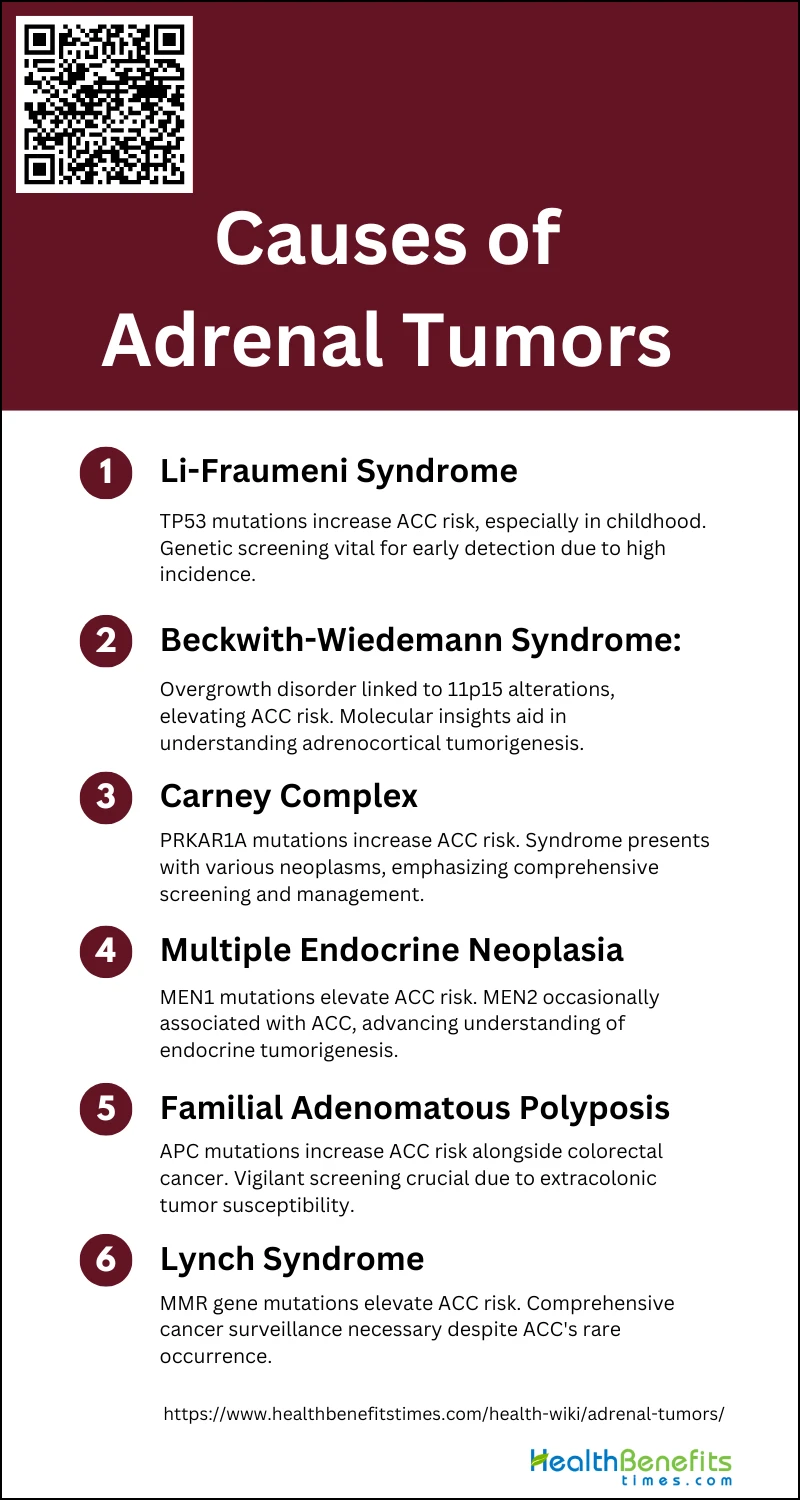
Causes and Risk Factors of Adrenal Tumors
Understanding the underlying causes and risk factors is crucial for early detection and effective management of these tumors. Below is a list of Causes and Risk Factors of Adrenal Tumors:
1. Li-Fraumeni Syndrome
Li-Fraumeni syndrome (LFS) is a hereditary disorder characterized by a predisposition to a variety of cancers, including adrenocortical carcinoma (ACC). This syndrome is caused by germline mutations in the TP53 gene, which plays a crucial role in regulating cell division and preventing tumor formation. Individuals with LFS have a significantly higher risk of developing ACC, particularly in childhood, accounting for 50-80% of pediatric cases. The spectrum of cancers associated with LFS also includes premenopausal breast cancer, soft-tissue sarcomas, osteosarcomas, and central nervous system tumors. The high incidence of ACC in LFS patients underscores the importance of genetic screening and early detection strategies.
2. Beckwith-Wiedemann Syndrome
Beckwith-Wiedemann syndrome (BWS) is an overgrowth disorder that increases the risk of developing various tumors, including adrenocortical carcinoma (ACC). BWS is typically caused by genetic or epigenetic alterations at the 11p15 locus, leading to the overexpression of growth-promoting factors and the loss of tumor suppressor gene function. The classical tumor spectrum of BWS includes embryonal tumors and childhood ACC, making it a significant risk factor for adrenal tumors in pediatric patients. The study of BWS has provided valuable insights into the molecular mechanisms underlying adrenocortical tumorigenesis, particularly the role of the 11p15 locus.
3. Carney Complex
Carney complex (CNC) is a rare genetic syndrome that predisposes individuals to multiple neoplasms, including adrenocortical tumors. CNC is primarily caused by germline mutations in the PRKAR1A gene, which encodes a regulatory subunit of protein kinase A. This syndrome is responsible for the majority of primary pigmented nodular adrenal diseases and is occasionally associated with adrenocortical carcinoma (ACC). Other manifestations of CNC include cardiac and cutaneous myxomas, lentiginosis, and various endocrine and non-endocrine tumors. The genetic and clinical features of CNC highlight the importance of comprehensive screening and management strategies for affected individuals.
4. Multiple Endocrine Neoplasia
Multiple endocrine neoplasia (MEN) is a group of hereditary disorders characterized by the development of tumors in multiple endocrine glands. MEN type 1 (MEN1) is associated with mutations in the MEN1 gene, which encodes the tumor suppressor protein menin. Patients with MEN1 are at increased risk of developing adrenocortical tumors, among other endocrine neoplasms4. MEN type 2 (MEN2), caused by mutations in the RET proto-oncogene, predisposes individuals to medullary thyroid cancer, pheochromocytoma, and parathyroid hyperplasia, with occasional reports of adrenocortical carcinoma (ACC). The study of MEN syndromes has provided significant insights into the genetic and molecular mechanisms of endocrine tumorigenesis.
5. Familial Adenomatous Polyposis
Familial adenomatous polyposis (FAP) is an inherited disorder characterized by the development of numerous polyps in the colon and rectum, with a high risk of progressing to colorectal cancer. FAP is caused by mutations in the APC gene, which plays a critical role in regulating cell growth and apoptosis. Although primarily associated with colorectal cancer, FAP patients also have an increased risk of developing other malignancies, including adrenocortical carcinoma (ACC). The association between FAP and ACC underscores the importance of vigilant screening and management of extracolonic tumors in FAP patients.
6. Lynch Syndrome
Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), is an inherited disorder that increases the risk of various cancers, including colorectal, endometrial, and adrenocortical carcinoma (ACC). Lynch syndrome is caused by germline mutations in mismatch repair (MMR) genes, such as MLH1, MSH2, MSH6, and PMS2, leading to microsatellite instability and increased cancer susceptibility. Although ACC is a rare manifestation of Lynch syndrome, its occurrence highlights the need for comprehensive cancer surveillance in affected individuals. The study of Lynch syndrome has provided valuable insights into the role of MMR genes in tumorigenesis and the importance of genetic counseling and testing.
Sign and Symptoms of Adrenal Tumors
It can manifest through a variety of signs and symptoms, often impacting bodily functions and overall health. These growths on the adrenal glands may cause hormonal imbalances and physical changes. Below is a list detailing the common indicators that may suggest of Sign and Symptoms of Adrenal Tumors:
- Abdominal pain
- Back pain
- Feeling of fullness in your belly
- Muscle cramps
- Weakness
- Headaches
- Excess facial or body hair (hirsutism)
- Newly elevated blood sugar (diabetes)
- High blood pressure
- Low potassium (hypokalemia)
- Unexplained weight loss
- Unexplained weight gain
- Fast heartbeat
- Enlarged breasts
- Enlarged penis or clitoris
- Low sex drive (low libido)
- Anxiety
- Panic attacks
Diagnosis of Adrenal Tumors
The diagnosis of adrenal tumors is a crucial process that requires a combination of clinical assessment, imaging techniques, and laboratory tests. Accurate identification of these growths is essential for determining the appropriate treatment plan and prognosis. In the following sections, we will outline the key steps involved in the diagnostic approach.
1. Physical Exam
A thorough physical examination is essential in the initial assessment of adrenal tumors. This includes evaluating the patient for signs and symptoms of hormone excess, such as hypertension, weight gain, and virilization. Physical findings may provide clues to the functional status of the tumor, such as Cushing’s syndrome or pheochromocytoma. However, physical examination alone is often insufficient to diagnose adrenal tumors definitively, necessitating further diagnostic tests.
2. Imaging Studies (CT, MRI, etc.)
Imaging studies play a crucial role in the diagnosis and characterization of adrenal tumors. Computed tomography (CT) and magnetic resonance imaging (MRI) are the primary modalities used. CT scans, particularly unenhanced CT with attenuation values, help differentiate benign adenomas from malignant lesions. MRI, with its superior soft-tissue contrast, is useful for further characterization when CT results are inconclusive. Functional imaging, such as FDG-PET, can also be employed to assess metabolic activity and malignancy risk.
3. Blood Tests
Blood tests are vital for evaluating the hormonal activity of adrenal tumors. These tests include measurements of cortisol, aldosterone, and catecholamines, among others. Elevated levels of these hormones can indicate functional tumors such as Cushing’s syndrome, Conn’s syndrome, or pheochromocytoma. Baseline hormonal evaluations, including serum DHEAS, can provide additional information on the likelihood of malignancy.
4. Urinalysis (Urine Tests)
Urinalysis, particularly urinary steroid profiling, is a valuable tool in differentiating between benign and malignant adrenal tumors. Gas chromatography/mass-spectrometry (GC/MS) can identify specific steroid metabolites that are elevated in conditions like adrenal cortical carcinoma (ACC). This method has shown high sensitivity and specificity in distinguishing ACC from benign adrenal masses, making it a useful diagnostic adjunct.
5. Biopsy
Adrenal biopsy, specifically adrenal core biopsy, can provide definitive histological diagnosis. This procedure is particularly useful when imaging and biochemical tests are inconclusive. Studies have shown high diagnostic accuracy for adrenal core biopsy, with sensitivity and specificity rates exceeding 90%. However, the procedure carries risks such as infection and hemorrhage, and its use is generally reserved for cases where malignancy is strongly suspected or when metastasis needs to be confirmed.
6. Molecular Testing
Molecular testing, including genetic and immunohistochemical analyses, is increasingly being used to diagnose and classify adrenal tumors. These tests can identify specific genetic mutations and protein expressions associated with malignancy. For instance, immunohistochemical markers like keratin, vimentin, and chromogranin a can help differentiate between various types of adrenal tumors. Molecular testing provides additional diagnostic precision, particularly in complex cases.
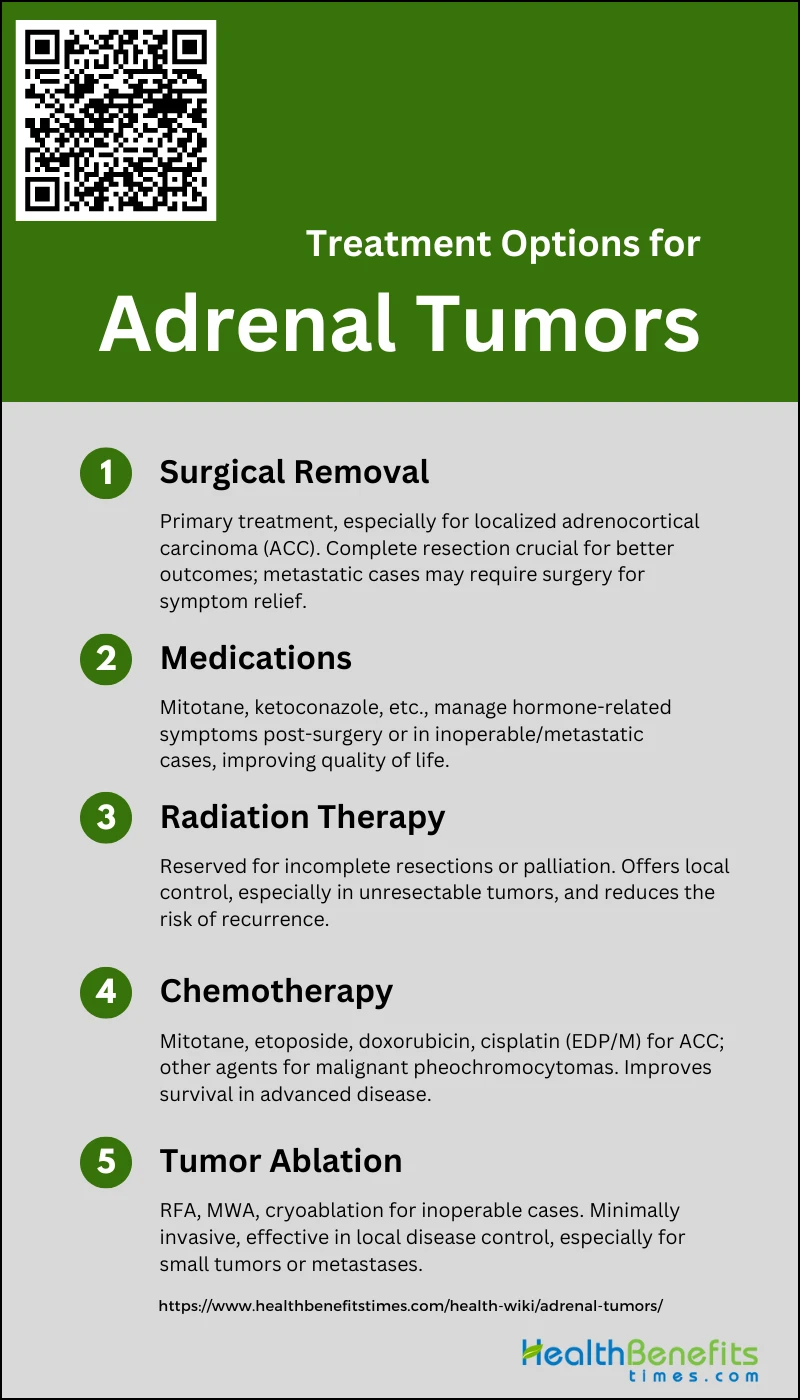
Treatment Options for Adrenal Tumors
Adrenal tumors present a unique set of challenges, but fortunately, there are multiple treatment options available to manage this condition. Depending on the type and stage of the tumor, patients can explore a variety of medical interventions. Here is a list of the most common treatment options for adrenal tumors:
1. Surgical Removal of the Tumor
Surgical removal is the primary treatment for adrenal tumors, particularly adrenocortical carcinoma (ACC). Complete resection by an experienced surgeon offers the best chance for a cure, especially in localized stages (I-III) of ACC. The goal is to achieve an en-bloc resection to avoid tumor spillage, which can lead to recurrence. Studies have shown that patients who undergo complete surgical removal have significantly better outcomes compared to those with incomplete resections or inoperable tumors. In cases of metastatic disease, surgery may still be considered for local control or symptom relief.
2. Medications to Manage Symptoms
Medications play a crucial role in managing symptoms associated with adrenal tumors, particularly those that secrete excess hormones. Mitotane is commonly used for its adrenolytic effects and is often administered post-surgery to reduce the risk of recurrence. Other medications like ketoconazole, metyrapone, and etomidate are used to control hormone production in cases where surgery is not feasible or in metastatic disease. These medications help manage symptoms such as Cushing’s syndrome, virilization, and hypertension, thereby improving the quality of life for patients.
3. Radiation Therapy
Radiation therapy is generally reserved for cases where surgical resection is incomplete or not possible. It is particularly useful for local control of unresectable tumors and for palliation of symptoms such as pain from bone metastases. Although ACC is traditionally considered resistant to radiation, recent studies suggest that it can provide significant local relief and improve survival in selected cases. Radiation therapy is also considered as an adjuvant treatment post-surgery to reduce the risk of local recurrence.
4. Chemotherapy for Malignant Tumors
Chemotherapy is typically used for advanced or metastatic adrenal tumors that are not amenable to surgical resection. The most effective regimen for ACC includes a combination of mitotane, etoposide, doxorubicin, and cisplatin (EDP/M), which has shown response rates up to 50% in clinical trials. Other chemotherapeutic agents like vincristine, dacarbazine, and cyclophosphamide are used for malignant pheochromocytomas. Despite its limited efficacy, chemotherapy remains a critical option for managing advanced disease and improving survival rates.
5. Tumor Ablation
Tumor ablation techniques such as radiofrequency ablation (RFA), microwave ablation (MWA), and cryoablation are increasingly used for patients who are not candidates for surgery. These minimally invasive procedures are guided by imaging techniques and are effective in controlling local disease, especially for small tumors or isolated metastases. Ablation offers a safer alternative with fewer complications and can be repeated if necessary. It is particularly beneficial for patients with multiple comorbidities or those who refuse surgery.